Phlebitis in Pregnancy: Symptoms and Treatment


Reviewed and approved by the nurse Leidy Mora Molina
Phlebitis in pregnancy is a common problem. In many cases, there are alterations in women’s veins when they’re between 20 and 25 years old, but not pregnant. But, as these aren’t always visible, they’re sometimes detected during pregnancy.
The point is that this condition can have serious consequences. Phlebitis in pregnancy must be treated in time in order to prevent complications such as thrombosis or even pulmonary embolism.
What is phlebitis?
Phlebitis is the inflammation of the veins. Or, more precisely, of the walls of a vein.
Sometimes, this is associated with the formation of a clot in the same area. In such cases, we’re speaking of thrombophlebitis.
Most commonly, this problem occurs in the legs, since circulation is from the feet to the heart. Prolonged immobility is also a triggering factor.
The main risk factors for developing this disease are pregnancy, advanced age, contraceptive use, and excess weight. The greatest risk is that a thrombus may form and lead to a pulmonary embolism.
Discover: Tips to Help Relieve Varicose Vein Pain
Phlebitis in pregnancy
Phlebitis in pregnancy is common, due to the fact that pregnancy itself induces greater coagulability in the blood. Also, the pregnant woman’s body produces more platelets. This leads to a greater risk of blood clots.
On the other hand, the enlargement of the uterus is a factor that compresses venous return and hinders normal circulation. The risk of phlebitis in pregnancy is higher in mothers who need to rest.
The disorder can be of 2 types:
- Superficial: If it takes place just below the skin. It’s rarely dangerous.
- Deep: If it occurs in deeper, larger diameter veins. This is considered a medical emergency because of the danger involved. It’s also known as deep vein thrombosis.
Symptoms
Symptoms of phlebitis in pregnancy vary, depending on whether the condition is superficial or deep. In the case of superficial phlebitis, the main signs are as follows:
- Increase in vein volume, detectable by palpation
- Reddening of the skin (erythema)
- Pain and heat in the area
- Fever
If phlebitis in pregnancy is deep, the symptoms are as follows:
- Pale or cyanotic (bluish) skin in the affected area
- Swelling in the leg (edema)
- Tachycardia
- A throbbing pain
- Fever
Many times, phlebitis in pregnancy doesn’t create symptoms. Likewise, the intensity of these symptoms doesn’t always make it possible to predict the outcome of the situation.
You may also be interested in: Description of Phlebitis and Its Symptoms and Treatment
Treatment of phlebitis in pregnancy
The main objective of treatment for phlebitis in pregnancy is to dissolve the clot that has formed and prevent the formation of new ones. Low molecular weight heparin (LMWH) is usually injected. Other medications, such as warfarin, should be avoided in pregnant women.
If the phlebitis is superficial, a daily injection of LMWH is usually prescribed for 6 weeks. If it’s deep, treatment is extended to 12 weeks or more.
Nonsteroidal anti-inflammatory drugs, such as aspirin, are contraindicated. They create a risk of hemorrhage or malformations in the fetus.
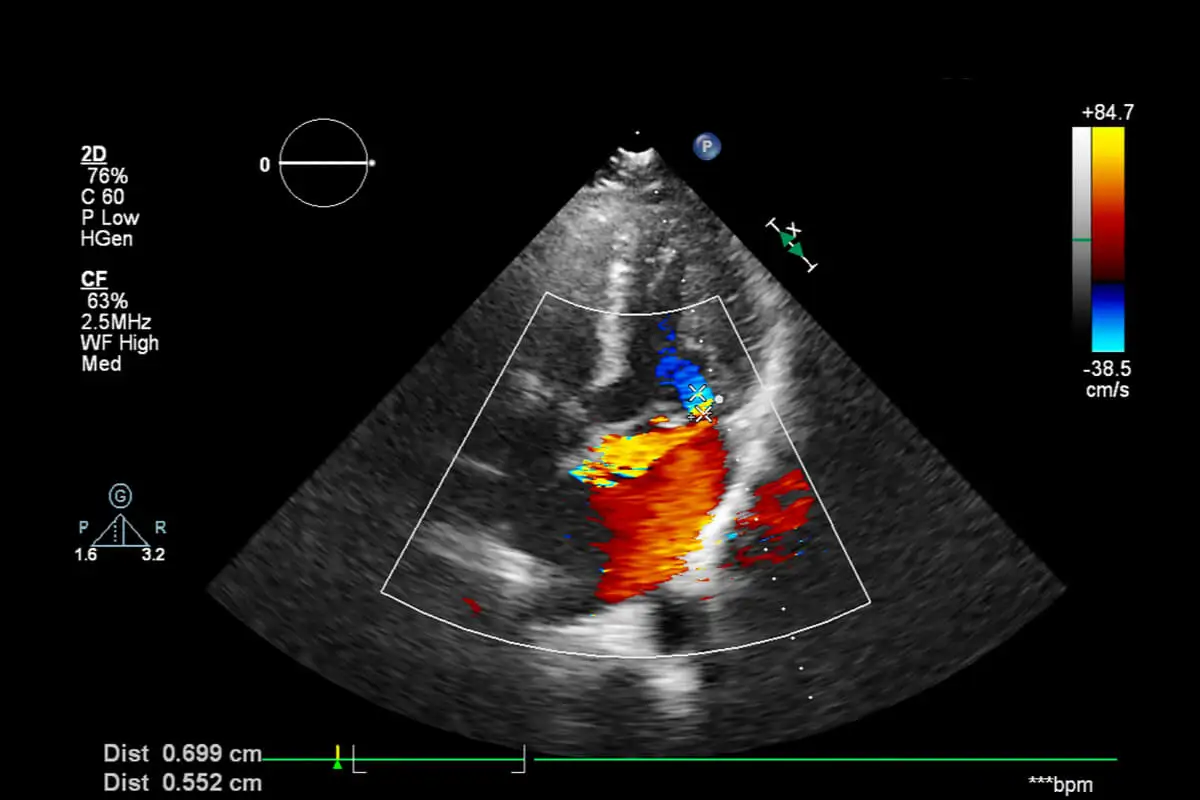
Several follow-up Doppler ultrasounds are recommended. They’re almost always performed every 15 days to monitor the evolution. In addition, the doctor prescribes type 3 compression stockings.
If, after applying these measures, new clots appear, then surgery will be necessary. This consists of placing a filter in the inferior vena cava, beyond the renal vessels. This measure prevents clots from reaching vital organs.
Tips and recommendations to follow
There are some simple measures that help prevent phlebitis in pregnancy. The first is to stay active during pregnancy.
A daily 20-minute walk or swimming is sufficient.
Other appropriate measures are as follows:
- Don’t wear flat shoes or high-heeled shoes. It’s recommended that shoes have a heel of 4 centimeters, to promote circulation in the calf.
- Sleep on the left side. This helps to decompress the inferior vena cava, which affects all the veins in the pelvis and legs.
- Wear compression stockings during long trips. Also stand up every 2 hours to activate circulation.
Phlebitis in pregnancy shouldn’t be taken lightly when giving birth. In fact, most thrombi develop during the postpartum period and the risk is highest at 6 weeks.
Caesarean section increases the danger.
If a pregnant woman feels a cramp-like pain in her leg and it doesn’t go away, especially if there’s redness, swelling or heat, then she should see a doctor immediately. Phlebitis in pregnancy is a serious condition.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- Ortiz, P., Javier, J. J., & Carvalho, R. (2013). Patología del sistema venoso superficial. Tromboflebitis, cuando anticoagular. Revisión del tema. Revisión de protocolos de tratamientos. Biomedicina, 8(3), 16-23.
- Gil, D. (2007). Embolia pulmonar. Rev. Méd. Clín. Condes, 103-109.
- Minetti, A., Haberstich, R., Feugeas, O., & Langer, B. (2007). Accidentes tromboembólicos venosos y embarazo. EMC-Ginecología-Obstetricia, 43(4), 1-13.
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








