Pulmonary Embolism: Symptoms and Treatment

Pulmonary embolism is a serious and relatively frequent problem. Experts estimate that it occurs in one in every 1,000 people per year. However, they think this rate might really be higher, since not all cases receive medical attention.
Pulmonary embolism occurs when a mass, generally a blood clot, obstructs blood flow to the lungs. Although a blood clot is the most common trigger, other culprits could be a fat or air embolism.
Pulmonary embolism can be fatal. It’s currently estimated that between 8% and 10% of patients with the condition die. The severity of each case is determined by the size of the obstructed artery, as well as the amount of lung tissue affected.
What is pulmonary embolism?
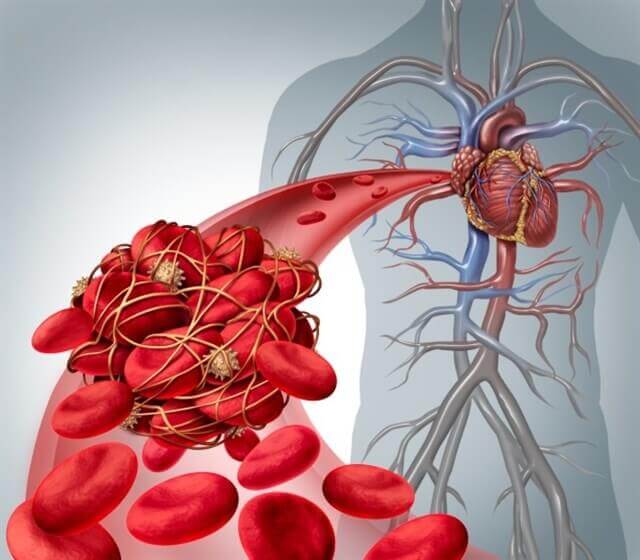
To put it simply, pulmonary embolism occurs suddenly due to obstruction of a pulmonary artery. This generally occurs when pieces of a venous thrombosis separate and travel, becoming lodged in an artery in the lungs.
Doctors divide pulmonary embolism into two main groups, according to severity. They are:
- High risk: Occurs when the patient has low blood pressure or experiences shock. The premature mortality rate in these cases is at least 15%.
- Normal blood pressure: Blood pressure is normal in these cases. It includes two subgroups:
- Low risk, which generally only requires an outpatient treatment.
- Heightened risk of complications, which requires urgent treatment and hospitalization.
Causes
The majority of pulmonary embolism cases are a secondary condition related to triggering risk factors. This means that they are a result of another health problem. The main risk factors are:
- Injuries to the legs
- Spinal damage
- Major traumatic injuries
- Major surgery
Another factor that can trigger pulmonary embolism is cancer. Lung cancer, pancreatic cancer, and cancers of the central nervous system are the most likely to causes complications involving thromboses. It’s the same situation with gastrointestinal tumors and blood neoplasms.
The hereditary component also has a major influence, although it’s not the determining factor. Pulmonary embolism is more common in women who take oral birth control. Additionally, pregnant women face a greater risk, especially during the third trimester and up to six weeks after giving birth.
Finally, the risk of pulmonary embolism is higher in those who have gone through in vitro fertilization, as well as in post menopausal women who are taking hormone replacement medications. The risk varies in the latter case, depending on which medications are being used.
Symptoms

Patients also commonly experience sudden, intense chest pain. The pain is felt behind the sternum, and is similar to the pain associated with heart attacks. The pain increases when the patient coughs and inhales, and doesn’t go away when the patient changes positions.
Also read: Chest Pains – Why Do They Happen
Additionally, the following symptoms are common:
- Syncope: loss of consciousness
- Dry or wet cough
- Hemoptysis: coughing up blood – this indicates that there is pulmonary infarction
- Tachypnea: increase in the breathing rate
- Tachycardia: increased heart rate
- Others such as paleness, cyanosis (bluish color of the skin), dizziness, fever, sweating, and disorientation.
You might be interested in: The Relationship Between Tachycardia and Anxiety
Treatment
Pulmonary embolism is diagnosed using a combination of clinical suspicion, diagnostic imaging, and D-dimer blood test. The patient’s symptoms determine the suspicion of pulmonary embolism. Chest X-ray, electrocardiogram, and a blood gas test serve as support when making a diagnosis.
Anticoagulants are the main course of treatment. At first, they are administered parenterally (intravenous, intramuscular, or subcutaneous), followed by subsequent oral administration.
If doctors detect and treat the condition in time, the patient’s prognosis is good. In 3.8% of cases the embolisms become chronic. Over the past several years, the number of patients who die while hospitalized for pulmonary embolism has decreased considerably.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- Konstantinides, S., Torbicki, A., Agnelli, G., Danchin, N., Fitzmaurice, D., Galiè, N., … & Kucher, N. (2015). Guía de práctica clínica de la ESC 2014 sobre el diagnóstico y el tratamiento de la embolia pulmonar aguda. Revista Española de Cardiología, 68(1), 64-e1.
- Golin, V., & Bedrikow, R. (2000). Embolia pulmonar. Revista Brasileira de Medicina.
- Gabriel, F., Labiós, M., Ferreres, J., & Ibáñez, L. (2013). Clasificación y tratamiento de la embolia pulmonar aguda. Angiología. https://doi.org/10.1016/j.angio.2012.12.002
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








