Surgical Menopause: What Is It and What Are Its Consequences?


Reviewed and approved by the nurse Leidy Mora Molina
Surgical menopause is a process that occurs in women after an operation to remove the ovaries. It is similar to natural menopause, only that it occurs at a still fertile age.
As a result, some changes occur in the body, manifesting various symptoms:
- Hot flashes
- Sweating
- Irritability
- Sleep disturbances
Menopause is a natural process in the body
Menopause is a process that women go through. It has to do with the cessation of egg production and a progressive decrease in sex hormone levels.
The age at which menopause begins may vary from person to person. In some women, it begins around the age of 45 and the stages can extend over a period of several years.
During this period, three phases are identified:
- Premenopause: the first symptoms appear due to the reduction of ovarian activity.
- Menopause: marked by the definitive disappearance of menstruation.
- Postmenopause: various symptoms appear, all of which are related to the drop in estrogen levels.
Like this article? You may also enjoy reading: 7 Tricks to Avoid Gaining Weight When You Reach Menopause
What is surgical menopause?
Unlike the previous one, surgical menopause, also called iatrogenic menopause, does not occur due to natural causes. It can happen at any age, that is, in women who are still able to conceive.
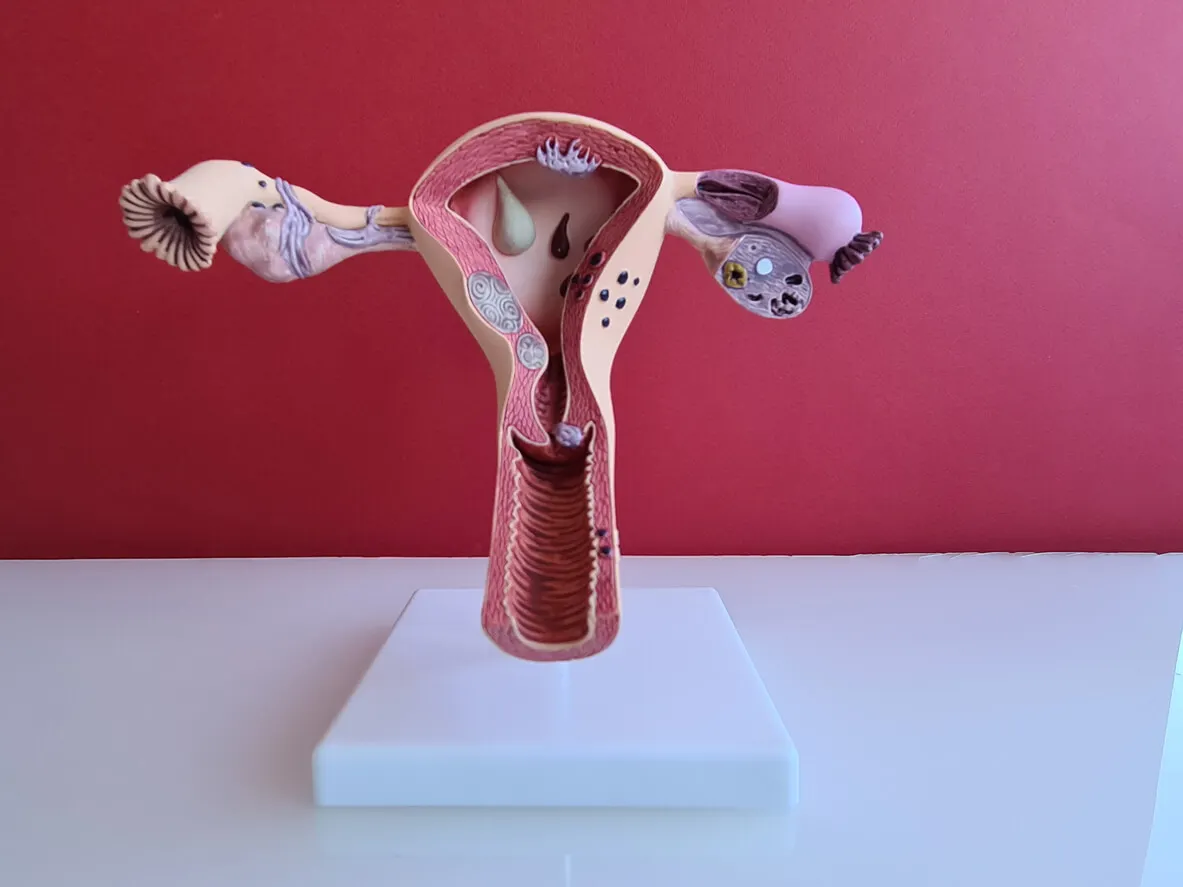
As its name implies, it is the consequence of a surgical intervention performed to remove the ovaries, called a bilateral ovariectomy or oophorectomy, which is the removal of the ovaries. This may be required for a variety of reasons:
- Cancer
- Endometriosis
- Abscesses in the fallopian tubes or ovaries
However, if an operation is performed to remove the uterus, but the ovaries (one or both) are left behind, the woman will have natural menopause, at the appropriate age. In other words, after the hysterectomy, menstruation will cease, but the ovarian function will allow estrogen production to continue.
It should be clarified that sometimes bilateral oophorectomy is performed together with hysterectomy, as a prophylactic measure to prevent cancer. In other words, healthy ovaries are removed. According to research, this can occur in 40-55% of cases.
The initial symptoms of surgical menopause
Once the oophorectomy is performed, some symptoms begin to appear. And although they are similar to those that occur when the process occurs naturally with age, in surgical menopause some appear from the first day after the operation.
In this order of ideas, among the symptoms of menopause that can appear immediately we can find the following:
- Dizziness
- Depression
- Irritability
- Headaches
- Hot flashes
- Sleep disorders
- Anxiety and nervousness.
- Excessive sweating (hyperhidrosis).
We think you may be interested in reading this, too: World Menopause Day: Let’s Give it the Importance it Deserves
The consequences of surgical menopause
Gradually, there are going to be other consequences of surgical menopause, because estrogen levels decrease. As occurs in the case of natural menopause, a person’s risk of developing several conditions increases. Let’s take a look at what they are.
Osteoporosis
Although estrogen, together with progesterone, are the main female sex hormones, they are also related to other functions in the body. In this sense, they have an effect on the bone system.
Therefore, when their levels decrease, bones become more fragile, increasing the risk of suffering fractures. According to studies, there are other factors that influence the onset of osteoporosis, such as family history, calcium intake, physical activity, obesity, and smoking.
Increased cholesterol and cardiovascular risk
Estrogen is also closely related to cholesterol. Thus, when the levels of this hormone increase, the levels of HDL cholesterol (or good cholesterol) also increase and those of LDL (bad cholesterol) are reduced.
According to research, a person’s cardiovascular risk increases with surgical menopause. Diseases such as atherosclerosis appear, as well as the possibility of suffering strokes and myocardial infarction.
Decreased sexual desire
According to the results of a study, in women with surgical menopause due to bilateral oophorectomy, with or without hysterectomy, the prevalence of hypoactive sexual desire disorder (HSDD) is higher.
Vaginal dryness
Another consequence due to the decrease in estrogen levels is that the vagina becomes less lubricated. It even changes the pH, which also affects the vaginal microbiota.
Other bodily changes
In addition to the above, low estrogen modifies the levels of collagen and elastin, causing their production to decrease. As a result, the skin loses moisture and shine, resulting in more wrinkles. Likewise, the nails may become brittle, and the possibility of developing alopecia increases.
Emtional disorders and depression
Due to menopause, women are more prone to suffer from mood disorders and various psychological problems, including depression, anxiety, irritability, nervousness, memory loss, and decreased concentration.
Treatment of surgical menopause
The aforementioned disorders can significantly affect a woman’s quality of life. Therefore, in order to reduce, avoid or prevent such symptoms and consequences, different types of treatment for surgical menopause are applied.

Like this article? You may also like to read: How To Take Care of Yourself During Menopause
Hormone replacement therapy (HRT)
Also called estrogen replacement therapy, it seeks to compensate for what the ovaries would normally produce. It’s applied in various ways, either with patches or orally (tablets).
These replacement hormones help to reduce symptoms, protect against osteoporosis, and prevent cardiovascular problems. They also reduce the frequency and intensity of hot flashes, collagen loss, and vaginal dryness.
However, HRT is considered to carry certain risks. In this regard, some studies indicate that it may increase the risk of stroke, venous thromboembolic disease, and breast cancer.
Other pharmacological treatments
Other treatments, alternative or complementary to hormone replacement, include the following options:
- Calcium and vitamin D supplements to prevent osteoporosis.
- Antidepressants and anticonvulsants for hot flashes and anxiety.
- Antihypertensives in the case of developing arterial hypertension.
Phytotherapy
Phytotherapy treatment for surgical menopause involves the use of extracts of various plant species, such as black cohosh, soybeans, red clover, butcher’s broom, red vine, olive leaf, and garlic.
They may have antioxidant, cardioprotective, and neuroprotective effects, helping to alleviate musculoskeletal disorders, memory loss, and hot flashes. According to studies, some plants have shown efficacy in alleviating certain symptoms.
However, more research is still needed in this regard.
Healthy lifestyle
Finally, a healthy lifestyle is recommended, with a diet rich in calcium, regular physical activity, striving to maintain a healthy weight, sunbathing in moderation (to maintain vitamin D levels), and avoiding smoking and excessive alcohol.
You are not alone if you’ve gone through a surgical menopause
Coping with the consequences of surgical menopause can be difficult for some women, as it affects their sex life and health. However, being able to count on help is valuable in these circumstances.
First of all, there is the family, the couple, and friends. Also, you should know that there are also support groups of people who have gone through the same situation and who meet to share their experiences.
However, if you feel that you are going through a difficult situation, do not hesitate to go to therapy with a mental health professional. Also, don’t forget to follow the doctor’s recommendations to the letter, as well as to attend all of your scheduled checkups.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- Alba Maldonado J. Trastorno de Ansiedad y menopausia quirúrgica Universitas Médica. 2007; 48(3): 325-333.
- Bolaños Chaves B, Ortega Muñoz E. Riesgo cardiovascular asociado a menopausia. Revista Médica Sinergia. 202; 6(1): e629.
- Ceinos Arcones M, Acosta Estévez E, Martín Perpiñán C, et al. Factores de riesgo en relación con la osteoporosis y la edad de presentación de la menopausia en población general. Atención Primaria. 1999; 24(3): 140 – 144.
- Cornellana Puigarnau M. Hypoactive sexual desire disorder in surgical menopause. Folia Clinica en Obstetricia y Ginecologia. 2008; 73: 36-39.
- Couto Núñez D, Nápoles Méndez D, Mustelier Ferrer H. Menopause surgically induced. MEDISAN. 2012; 16(12): 1906-1914.
- Gallego M, González A, Méndez S, et al. La fitoterapia en el tratamiento de los síntomas de la menopausia. Gaceta Médica de Bilbao. 2009; 106(2): 61-67.
- Jacoby V, Grady D, Wactawski-Wende J, et al. Oophorectomy vs ovarian conservation with hysterectomy: cardiovascular disease, hip fracture, and cancer in the Women’s Health Initiative Observational Study. Arch Intern Med. 2011; 171(8): 760-768.
- Lara TH, Bravo LM, Meléndez MJD, et al. Depresión mayor y menopausia. Un estudio controlado. Rev Neurol Neurocir Psiquiat. 2002; 35(3): 138-143.
- Shuster L, Gostout B, Grossardt B, Rocca W. Prophylactic oophorectomy in premenopausal women and long-term health. Menopause International. 2008; 14(3): 111-116.
- Urrutia M, Araya A, Padilla O. Sexualidad e histerectomía: diferencias entre un grupo de mujeres con y sin ooforectomía. Rev. chil. obstet. ginecol. 2011; 76(3): 138-146.
- Yuschak S. Tipos de ooforectomía e indicaciones en cáncer de mama. Rev Arg Mastol 2005; 24(83):142-158.
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








