Embryo Transfer: How and Why Is It Performed?
Embryo transfer is one of the critical points in assisted reproduction processes. It’s the final step in in vitro fertilization (IVF) treatments performed conventionally or by intracytoplasmic sperm injection.
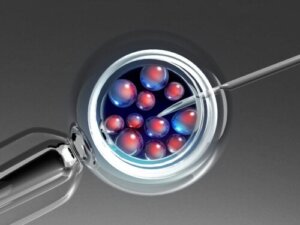
In assisted reproduction, fertilization of the egg and sperm is performed in a laboratory. This should result in embryos suitable for implantation in a woman’s uterus. This particular step is called embryo transfer.
In order for it to be successful, the right moment must be chosen. The embryo must have reached a certain stage of development and the woman’s uterus must be ready to receive it.
Defining embryo transfer
Embryo transfer is the process by which embryos generated in a laboratory are placed into the woman’s uterus. The hope is that the embryo will implant and result in pregnancy.
The success of embryo transfer depends on two factors. On the one hand, the quality of the embryos. On the other hand, the condition and receptivity of the endometrium. Both elements are decisive.
In addition, the process must be carried out at the right time and the technique must be applied in an appropriate manner. One of the most important steps is the verification that the embryo didn’t remain in the transfer cannula.
Read more: 15 Fertility Myths Heard by Specialists
Types of transfer
Embryo transfer is the last, and perhaps most decisive, step in in vitro fertilization (IVF). It doesn’t always take place immediately after fertilization has been achieved in the laboratory.
Sometimes embryos are vitrified. That is, they’re frozen for preservation and later use.
All this gives rise to two types of embryo transfer:
- Fresh: When the embryos are transferred without having been frozen.
- Deferred: When the embryos have been previously frozen. This is also called cryotransfer.

When is it carried out?
Before talking about the correct moment to carry out embryo transfer, let us remember what the stages of embryo development are. First, fertilization takes place, which is the actual union of the egg and the sperm. This is how the zygote is formed.
The zygote begins to divide. It gives rise to two cells; each of them divides into two others and so on.
On the third day, there are already eight cells and then we speak of the existence of an embryo. On the fourth day there’s a morula, which is a structure with a large number of cells compacted together.
Between the fifth and sixth day, the embryo reaches a stage called blastocyst. This is when there’s a structure with cells of different kinds that will form the fetus.
It’s usual for embryo transfer to be done when the embryo is at this stage.
A study carried out in 2009 found that there’s a greater probability of success when embryo transfer is carried out on the fifth day, with the embryo in the blastocyst stage. However, the subject is still under discussion.
How is it performed?
Embryo transfer is a simple, quick procedure that doesn’t require sedation. In some cases, it takes advantage of the woman’s natural menstrual cycle, when the female hormones prepare the endometrium for pregnancy.
Other times, the woman is prescribed medications to provoke changes favorable to pregnancy. Once the embryos are ready and the endometrium is prepared, the procedure is performed.
Usually the woman is asked to come with a full bladder and without makeup.
Abdominal ultrasound is used to advance the procedure. Once in the operating room, the following steps are taken:
- Placement of a sterile speculum in the vagina.
- Cleaning of the area with physiological saline solution.
- Cleaning of the cervix and aspiration of cervical mucus.
- Loading of the embryos in a catheter or transfer cannula.
- Introduction of the catheter through the vagina until it reaches the uterus.
- Slow deposition of the embryos in the uterus.
- Careful removal of the catheter.
- Verification that the embryos have not remained in the cannula.
What to keep in mind afterwards
Once the embryo transfer is completed, the woman must remain at rest in the clinic for 20 to 30 minutes. She can then go about her normal life, but is advised to do the following:
- Drink plenty of water.
- Not exert herself excessively.
- Avoid immersion baths, as they can cause infections.
- Avoid sexual intercourse until a pregnancy test is done.
If a successful pregnancy isn’t achieved, she can try again in the next cycle. More embryos will be available in the laboratory and these will be preserved until the woman reaches the end of her childbearing years.
Occasionally, slight bleeding is detected after the embryo transfer, but this shouldn’t be a cause for concern. It’s also possible to experience pain or discomfort similar to premenstrual pain.

What’s a simulated embryo transfer?
It’s very common for one or more simulated transfers to be performed before the actual transfer is carried out. This is a way for the doctor to perfect the technique and, in this way, increase the probability of success.
By means of the simulated embryo transfer, the professional is able to measure the length from the cervix to the area of the uterus that is to be reached. Possible obstacles to the procedure, such as a fibroid, are also detected.
There’s some disagreement among specialists on the subject. However, most agree that this type of simulation increases the success rate.
Read more: Can You Get Pregnant with Pre-Seminal Fluid?
A technique always in progress
In assisted reproduction, as in so many other cases, research is still ongoing. Although there are still some disagreements, there are enough studies that support embryo transfer at the blastocyst stage and not at the morula stage.
Until recently, the usual practice was to transfer several embryos. However, nowadays it’s considered more advisable to transfer a single embryo to avoid the risk of unwanted multiple pregnancies.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- Salas, S. P. (2021). Aspectos éticos respecto de embriones humanos producidos en el laboratorio. Revista médica de Chile, 149(4), 652-653.
- Guerif F, Lemseffer M, Bidault R, Gasnier O, Saussereau MH, Cadoret V, Jamet C, Royere D. Single Day 2 embryo versus blastocyst-stage transfer: a prospective study integrating fresh and frozen embryo transfers. Hum Reprod. 2009 May;24(5):1051-8. doi: 10.1093/humrep/dep018. Epub 2009 Feb 13. PMID: 19218575.
- De Acosta, O. M., & Valdés, N. A. (2020). Fertilización in vitro (FIV) y transferencia de embriones (TE) en el humano, consideraciones éticas, científicas y utilidad. Revista Cubana de Medicina, 24(8).
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








