Carotid Artery Disease: Causes and Treatment


Reviewed and approved by the doctor Leonardo Biolatto
The cardiovascular system is indispensable for the functioning, nutrition and maintenance of all the body’s organs. Several pathologies can compromise the health of arteries and veins. Are you interested in learning more about carotid artery disease? Here we’ll tell you all about it.
The carotid arteries are a pair of large-caliber arteries located on both sides of the neck. They are responsible for supplying blood from the aorta to the face, brain, and various cranial structures. At the encephalic level, they supply to the regions related to motor and sensory functions, as well as speech, thought and personality.
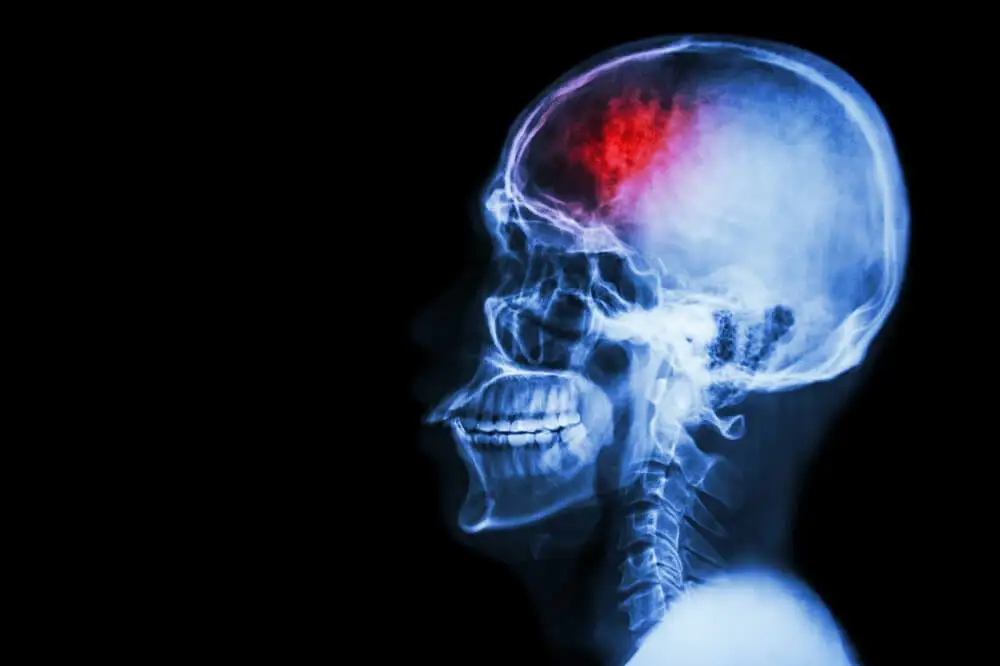
Carotid artery disease greatly increases the risk of cerebrovascular accidents (CVA). Studies estimate that this condition is responsible for more than 11% of the annual ischemic stroke cases in Argentina (article in Spanish).
What is carotid artery disease?
Carotid artery disease is also called carotid artery stenosis. It occurs when there’s a narrowing or blockage of these blood vessels.
Carotid occlusion is usually caused by the accumulation of cholesterol and the deposit of fatty substances in the walls of the carotid arteries. The formation of plaques in the blood vessels is referred to as atherosclerosis.
Vascular blockage reduces blood flow to the brain and increases the risk of an ischemic stroke. The latter occurs when there’s an occlusion or total interruption of the carotid blood supply. In this sense, the cessation of blood flow to the brain leaves the neurons without oxygen and they die.
Carotid artery disease has a pathophysiological basis similar to coronary artery disease, with myocardial infarction being the final outcome of the latter. On the other hand, carotid stenosis can affect one or both arteries and its early therapeutic approach improves quality of life.
Read more here: Cardiovascular Risk: How Does Diet and Exercise Help?
Common symptoms
In most cases, carotid artery disease evolves slowly and goes unnoticed in its early stages. In this sense, it’s common for this condition not to manifest any signs or symptoms until it has become severe.
Transient ischemic attacks are abrupt conditions that appear before the temporary occlusion of a small caliber cerebral vessel. The duration varies from a few minutes to several hours. The manifestations disappear completely within 24 hours, but their persistence leads to a diagnosis of stroke.
In both cases, the following symptoms can be found:
- Sudden weakness in a limb or half of the body
- Paralysis of an arm or leg on one side of the body
- The inability to perform certain movements
- Loss of the ability to coordinate movements
- Confusion, dizziness and severe headaches
- The loss of sensation in the face or body
- Numbness or paresthesias in the extremities
- Blurred vision or total loss of vision
- Difficulty in articulating words and speaking clearly
Upon evidence of any stroke symptoms, medical attention should be sought as soon as possible. This is a condition with a high risk of mortality that requires professional management.
Why does carotid artery disease occur?
Research affirms that the main cause of carotid artery disease is atherosclerosis. Atherosclerosis is caused by the accumulation of cholesterol, calcium, cellular debris and fibrous tissue in the walls of the blood vessels. The end result will be a plaque that obstructs the normal flow of blood in the artery.
In general, carotid vessel walls subject to this phenomenon tend to become harder over time, narrowing the vascular lumen. Thus, they won’t be able to maintain adequate flow to vital organs.
Risk factors
There are a variety of conditions that increase the likelihood of carotid artery disease. Most of the risk factors are similar to those for other cardiovascular conditions, among which are the following:
- Sedentary lifestyle
- Being male
- Sleep apnea
- Diabetes mellitus
- Arterial hypertension
- Obesity and being overweight
- Excessive alcohol intake
- Being Hispanic or African-American
- Tobacco or cigarette smoking
- Old age (over 65 years old)
- High levels of triglycerides and bad cholesterol (LDL)
- Family history of atherosclerosis and cardiovascular disease
Associated complications
Atherosclerotic carotid stenosis or occlusion causes about 30% of cerebrovascular ischemia, according to research (article in Spanish). This is a high-risk complication with a high mortality rate if not treated promptly.
Strokes due to carotid artery disease occur due to the following:
- Decreased blood supply
- Thrombi due to rupture of atherosclerotic plaques
- Clot formation and obstruction of the vascular lumen
How is carotid artery disease diagnosed?
Carotid artery disease is almost always diagnosed late, after experiencing some type of stroke. In this case, a detailed study of the trigger can help to identify carotid stenosis.
Similarly, during a thorough physical examination, it’s possible to detect certain findings that can guide the clinician to suspect carotid blockage. One sign of this pathology is the perception of an abnormal sound or murmur, similar to a whistling sound, during auscultation of the neck with the stethoscope.
In addition, the specialist usually evaluates the neurological, as well as the physical and mental capacities. On the other hand, several tests are very useful in the diagnosis of carotid artery disease:
- Ultrasound
- Cerebral angiography
- Magnetic resonance imaging (MRI)
- Computed tomography (CT) angiography

Medical treatment
The treatment of carotid stenosis is aimed at slowing the evolution and progression of the disease. The main goal is to prevent the outcome of a stroke. The therapeutic plan depends on the degree of occlusion and the general condition of the individual.
In the early detection of this condition, it’s necessary to start with lifestyle modifications. In this regard, it’s recommended to follow a healthy diet, exercise, lose weight, avoid smoking and reduce salt intake.
In mild to moderate cases, the specialist usually prescribes medication to control blood pressure and prevent the formation of atherosclerotic plaques. In addition, in the elderly, antiplatelet agents such as aspirin and anticoagulants may be prescribed.
On the other hand, in severe carotid artery disease or in people with a previous history of strokes, surgery is usually recommended. The approach options are as follows:
- Carotid endarterectomy: This is the first-choice procedure to eliminate blockage of the carotid arteries. It consists of vascular approach and dissection in order to remove the atherosclerotic plaque.
- Carotid angioplasty with stent placement: This is used in advanced cases that aren’t suitable for resolution by endarterectomy. During the procedure, a small balloon is inserted inside the blood vessel to expand it and then a mesh or stent is placed to prevent vascular narrowing.
Find out more: Stents in Arteries: Everything you Need to Know
A healthy lifestyle is key to preventing the disease
Carotid artery disease is a pathology associated with the formation of atherosclerotic plaques in these vessels and their consequent occlusion. The risk of mortality is high in people with unhealthy habits that accelerate the disease’s progression.
A balanced diet, as well as the practice of physical activities, greatly improve the quality of life and the long-term prognosis. If you have any concerns, don’t hesitate to consult your doctor.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- Sposata L. Enfermedad carotídea aterosclerótica extracraneal. Neurología Argentina. 2011; 3(1): 25-63.
- Consenso de Estenosis Carotídea. Rev. argent. cardiol. 2006; 74( 3 ): 160-174.
- Reina T, Martínez I. Las carótidas enfermas. Libro de salud cardiovascular. 2010; 4(1): 527- 535.
- Villaverde J, Gallardo F. La endarterectomía carotídea debe persistir como la técnica de elección para la mayoría de los pacientes con estenosis carotídea en la era endovascular. Sociedad Española de Angiología. 2016; 68(2):127-138.
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








