What Is a Macular Fold: Symptoms, Causes, and Treatments


Reviewed and approved by the nurse Leidy Mora Molina
A macular fold is a formation of extra tissue in the center of the retina. It’s not a very common condition. Sometimes it presents with mild symptoms. However, other times, it can affect a person’s vision.
The cause is not always known, although it’s associated with age-related degeneration. Most patients do not require treatment unless the person finds it difficult to perform activities.
What is a macular fold?
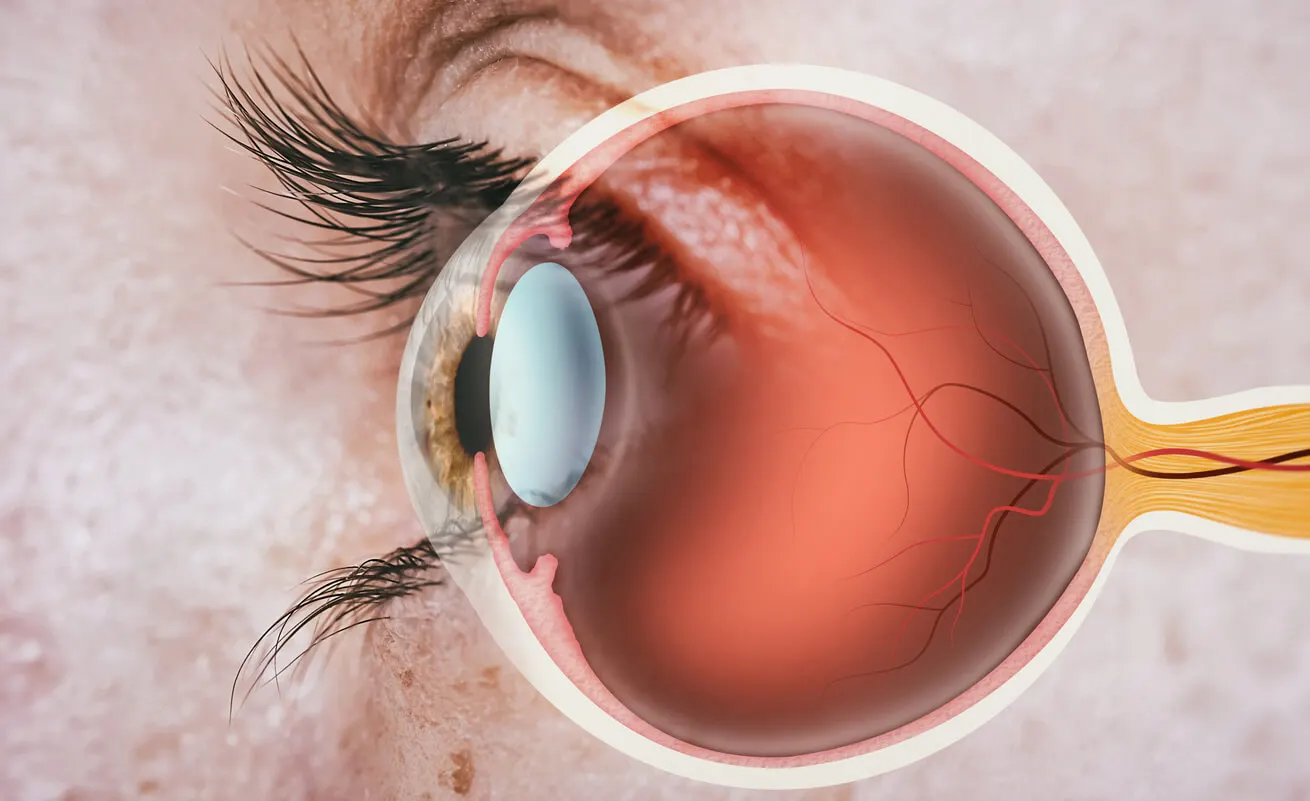
At the back of the eye is the retina. In particular, in the center of the retina is the macula, which is made up of special cells that react to light.
However, there are different conditions that can affect this area of the eye, diminishing our ability to perceive images. These include a macular hole, macular edema, and age-related macular degeneration.
On the other hand, cells inside the eye can grow. This causes the tissue to wrinkle, contract, or become tight, resulting in a scar membrane-like sheet or bulge.
This is called macular puckering or macular folding. It’s also known by other names:
- Epiretinal or preretinal membrane
- Cellophane retinopathy
- Wrinkles in the retina
We think you may be interested in reading this, too: The Keys to Good Visual Hygiene for Preventing Eye Damage
The symptoms of macular folds
In some people, there are no symptoms. In other cases, they are rather mild and don’t cause significant vision loss.
However, there may also be a distorted perception, making it difficult to perform daily activities. Among the most frequent symptoms of macular folding, the following can be mentioned:
- Blurred central vision
- Difficulty reading small print
- There may be difficulty in perceiving details
- Objects appear wavy (even straight lines)
- Sometimes, a gray or cloudy, even empty area can be noticed (like a blind spot_
Macular fold does not affect a person’s peripheral vision.
The causes of macular folds
Most of the time, the cause is not known. Among those that have been identified are the following:
- Aging: Over time, the vitreous humor of the eye may become compacted, separating from the retina. It may also stick together, causing scar tissue to form.
- Injury or disease, such as diabetes.
- Surgical intervention, such as retinal surgery or cataract surgery.
- Other causes, such as retinal tears or detachment or blood supply problems in the area.
There are also risk factors that increase the risk of macular folding. In this regard, inflammation inside the eye and uveitis stand out
Like this article? You may also like to read: Why Do we Find it Difficult to Maintain Eye Contact When Speaking?
How is the diagnosis made?
For the diagnosis, the ophthalmologist will place some drops in order to dilate the pupil. This will allow you to see inside using an apparatus called a ophthalmoscope.
If macular folding is suspected, an additional optical coherence tomography (OCT) scan may be performed, which scans the back of the eye, providing detailed images of the retina and macula.
Treatment options
In most cases, there are no or mild symptoms, so no treatment is required if a person’s vision is not affected. However, there are situations where glasses may be prescribed. It may also happen that the person who already uses optical correction may have to modify it.
Surgery is only recommended in some cases, when symptoms are more severe or disabling. In this regard, there are two possibilities:
- Vitrectomy: In this surgery, part of the vitreous humor and scar tissue is removed. It’s an outpatient process, which seeks to reduce or flatten the macula. It’s recommended when the cause is related to basic surgical procedures.
- Membranectomy: In this surgery the retinal membrane is removed. It can also be done on an outpatient basis. This is the usual procedure in the undesired consequences of cataract surgery or after uveitis.
Risks of surgeries
With surgery, it is possible that, in some cases, vision may improve, but it won’t be as good as before developing the fold. However, there are people who do not experience such improvement after the surgery.
In addition, as with any surgery, vitrectomies and membranectomies carry risks. These include the following:
- Cataracts
- Infections
- Hemorrhage
- Retinal detachment

Can macular folding be prevented?
Considering that the cause of this condition is not known in all cases, it’s not always possible to prevent or even stop macular folding from occurring. However, it is necessary to take precautions in people with diabetes or who have suffered from retinal detachment. This is also the case for those who have undergone cataract surgery.
Similarly, since age is one of the associated factors of this condition, it’s important to see an ophthalmologist regularly for eye examinations. This is the case if you suffer from macular folding to make sure it doesn’t get worse, and for early diagnosis.
It’s easier to treat a new macular fold than one that has been there for some time. It’s also possible that, in some cases, the problem may start in one eye and then affect the other eye.
A macular fold may grow back after removal, although this is not the most common occurrence.
When to see a doctor
Often, we experience certain strange phenomena in our vision, such as momentary blurring. If we go from a light place to a dark place, we may not see well.
However, if there are often problems of blurred vision, distortions, and difficulty in focusing on what’s in front of us, then it is better to see an ophthalmologist.
Meanwhile, when a macular fold is detected, there’s no need to be alarmed. Treatment is usually not necessary if the symptoms are mild. And whether this problem is present or not, whatever condition is affecting your vision shouldn’t be allowed to progress.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- American Academy of Ophthalmology. Pliegue macular. 2017. Documento en línea: disponible en: https://saeye.com/wp-content/uploads/handouts/spanish/Pliegue-macular.pdf
- Andre J, Hsu J. Surgical repair of macular fold after vitrectomy for bullous rhegmatogenous retinal detachment witkin. Retina. 2012; 32(8): 1666-1669.
- El-Amir A, Every S, Patel C. Repair of macular fold following retinal reattachment surgery. Clinical & Experimental Ophthalmology. 2007; 35: 791-792.
- Gómez Resa M, Mateo C. Manejo de los Pliegues maculares psotquirúrgicos. Rev. esp. investig. Oftalmol. 2013; 3(2): 102-105.
- Güemez-Sandoval E. Hermann von Helmholtz y el oftalmoscopio. Rev Mex Oftalmol. 2008; 82(1): 62-64.
- Molina Martín J. Evaluación anatómica, funcional e inmunohistoquímica de pacientes con membranas epirretinales idiopáticas. Universidad de Alicante, 2018.
- Rodríguez García A. Cirugía de catarata en uveítis. En Oftalmología en la opinión de los expertos. México: Garaitia Editores, 2011. Libro 7. Uveítis. 48-56.
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








