Vitreous Hemorrhage: Symptoms, Causes and Treatment

Reviewed and approved by the doctor Leonardo Biolatto
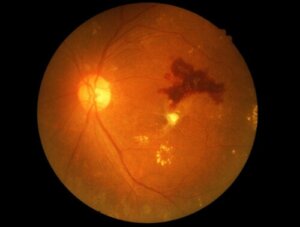
Vitreous hemorrhage is bleeding that occurs in the vitreous humor, a liquid, gel-like area between the inner surface of the retina and the posterior aspect of the lens. This causes sudden abnormalities in vision.
Experts estimate that it occurs in 7 out of every 10,000 people. It is also known as hemovitreal and can have different levels of severity. Sometimes it doesn’t require treatment and yet on other occasions it can require surgery.
Vitreous hemorrhage sometimes only causes blurred vision, although it also causes the appearance of spots floating in the visual field. In the most severe cases, it results in a complete loss of vision.
What is vitreous hemorrhage?
Vitreous hemorrhage is the presence of blood in a cavity of the eye that is filled with vitreous humor. The latter is a fluid composed of 99% water plus small amounts of collagen, hyaluronic acid, glucose, sodium, potassium, chlorine and proteins.
The vitreous humor occupies two-thirds of the total volume of the eye. Its appearance is transparent and gelatinous.
When blood is present, it loses its transparency and this hinders light penetration. Consequently, vision disturbances occur.
Vitreous hemorrhage can be of two types:
- Intravitreal: When bleeding occurs inside the vitreous cavity, in the space where the vitreous humor is. This is the disorder we are mentioning.
- Retrovitreal or subhyaloid: When it occurs in the space between the vitreous humor and the retina. It is usually classified in a different category than vitreous hemorrhage.
Read all about What Your Eye Color Says About You
Symptoms
The characteristic symptom of vitreous hemorrhage is loss of visual acuity in one eye only and without pain, which occurs suddenly and develops within a few minutes. Depending on the intensity of the bleeding, there’ll either be partial or total loss of normal vision.
Occasionally, affected people experience photopsias, which are flashes of light. They’re also known as ocular phosphenes.
Also, miodesopsias, which are small dark shapes floating in the visual field, may occur. They’re often called floaters.
In severe cases, vitreous hemorrhage can lead to glaucoma. This is due to the obstruction with blood of a natural drainage pathway of the eye, called the trabecular meshwork.
Causes of vitreous hemorrhage
Vitreous hemorrhage has many different causes. The most common is diabetic retinopathy, an eye disease caused by diabetes.
This pathology causes abnormal blood vessels to grow in the retina. They break easily and carry blood into the vitreous cavity.
Proliferative diabetic retinopathy (which promotes the growth of new abnormal blood vessels) is the cause of about 50% of cases of vitreous hemorrhage. The next 5 most common causes of this condition are as follows:
- Retinal detachment
- Detachment of the posterior vitreous
- Central retinal vein obstruction
- Hypertensive retinopathy
- Congenital retinoschisis
95% of spontaneous cases are due to these causes. The remaining 5% may be caused by inflammation (uveitis) or an ocular tumor. Vitreous hemorrhage can also be caused by trauma or surgery on the eye.
Read also: Everything You Need to Know About a Detached Retina
Diagnosis
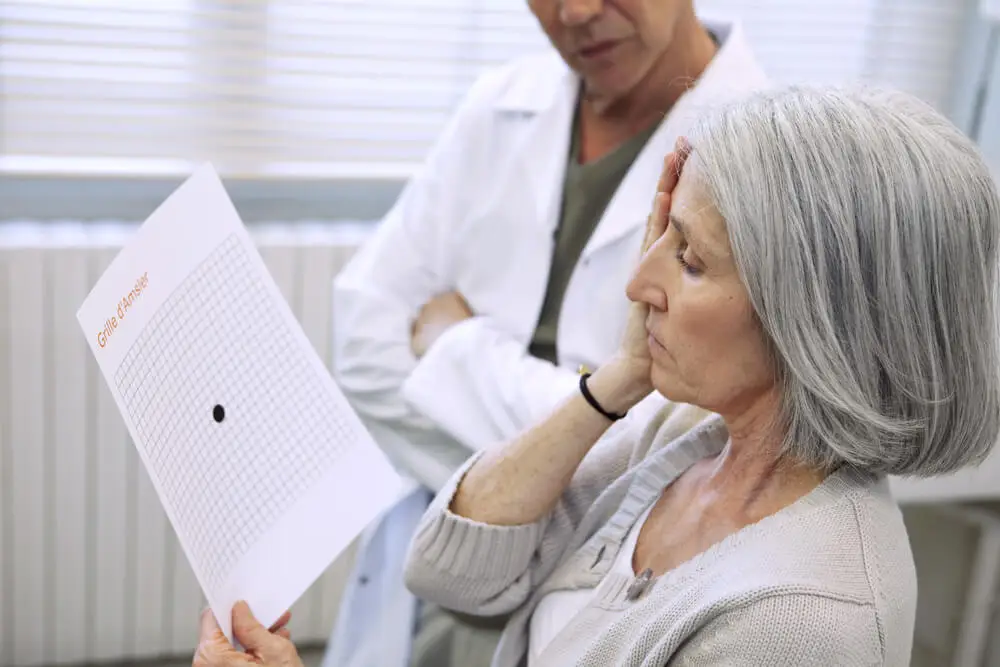
In principle, vitreous hemorrhage is diagnosed by talking with the patient and a thorough ophthalmological examination. This takes into account the fundus and visual acuity.
If the bleeding is very extensive, an ocular ultrasound may be ordered to rule out or confirm retinal detachment. Ocular pressure checks for glaucoma should also be performed.
In some cases, an x-ray or computed tomography (CT) scan is performed. Blood tests and examination of the other eye are also common.
Treatment of vitreous hemorrhage
Treatment for vitreous hemorrhage depends on the cause. A watchful waiting approach, i.e., nothing more than keeping the person under observation, is usual at first.
Many of these cases resolve spontaneously 2 to 3 months after the episode.
Measures such as the following may be recommended:
- Sleeping with the head raised. This helps to reduce the accumulation of blood in the eye.
- Not lifting heavy objects or doing strenuous activities.
- Avoiding the use of aspirin and anticoagulants.
- Have a follow-up ultrasound every 4 weeks.
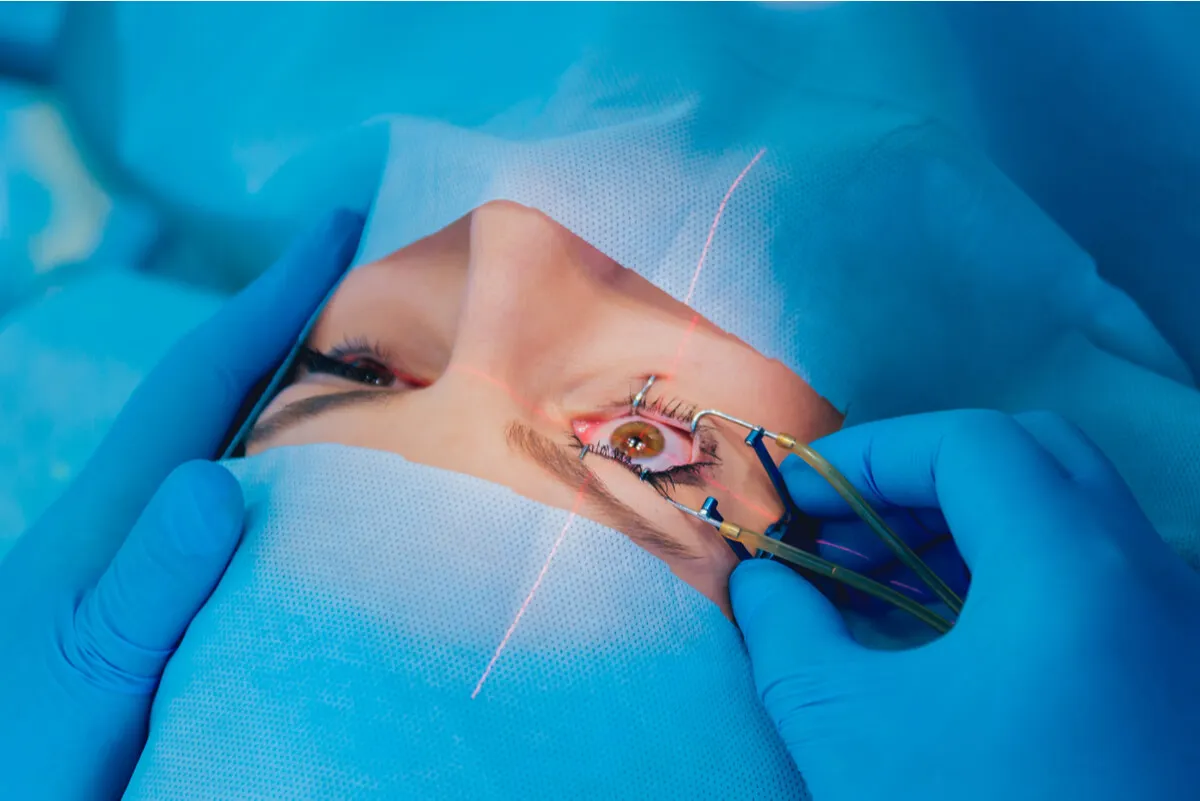
If the bleeding doesn’t spontaneously reabsorb or if there’s retinal involvement, surgery is necessary, This is called a vitrectomy. During this procedure, all of the vitreous humor is removed from the eye and replaced with a saltwater solution.
If the bleeding is very profuse, but there’s no retinal involvement, cryotherapy or laser treatment may be used. These procedures help stop the bleeding or remove the blood. A laser method called panretinal photocoagulation prevents rebleeding and reproliferation in cases of diabetic retinopathy.
Can it be prevented?
Vitreous hemorrhage cannot always be prevented, but there are some measures that help to reduce the risk. For example, visiting the ophthalmologist regularly, controlling the level of sugar in the blood if you have diabetes and protecting the eyes in activities that can put them at risk.
In case of symptoms of a vitreous hemorrhage, the best thing to do is to consult a doctor as soon as possible. If you have already been diagnosed with this condition, you should remain alert to any changes and always attend the periodic check-ups.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- Ferreiro, A. S., & Bellido, L. M. (2014). Hemorragia subhialoidea macular, tratada mediante ruptura de la hialoides posterior con láser YAG en un síndrome de Terson. Archivos de la Sociedad Española de Oftalmología, 89(2), 62-65.
- Padilla, J. S. (2016). Miodesopsias (o moscas flotantes). Revista Médica de Costa Rica y Centroamérica, 73(620), 525-527.
- Fernández, J. M. F., López, J. Á. F. V., Rodriguez, J. C., & Sánchez-Salorio, M. (1988). Tratamiento de la hemorragia vítrea diabética mediante criocoagulación panretiniana. Archivos de la Sociedad Española de Oftalmologia, 54(6), 819-828.
- Sarabia, César Pineda, Xóchitl Josefina Zarco Vite, and María Luisa Ruiz Morales. “Retinopatía diabética, una complicación descuidada.” Atención Familiar 25.2 (2018): 83-85.
- Alba-Linero, C., et al. “Vitrectomía diagnóstica: serie de casos en un centro de referencia.” Archivos de la Sociedad Española de Oftalmología 94.11 (2019): 529-535.
- Esmerado, C., et al. “Fotocoagulación panretiniana y tratamiento antiangiogénico en la retinopatía diabética proliferativa.” Annals d’oftalmologia: òrgan de les Societats d’Oftalmologia de Catalunya, Valencia i Balears 23.1 (2015): 5.
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








