Thyroid Eye Disease: Symptoms and Treatments


Written and verified by the biologist Samuel Antonio Sánchez Amador
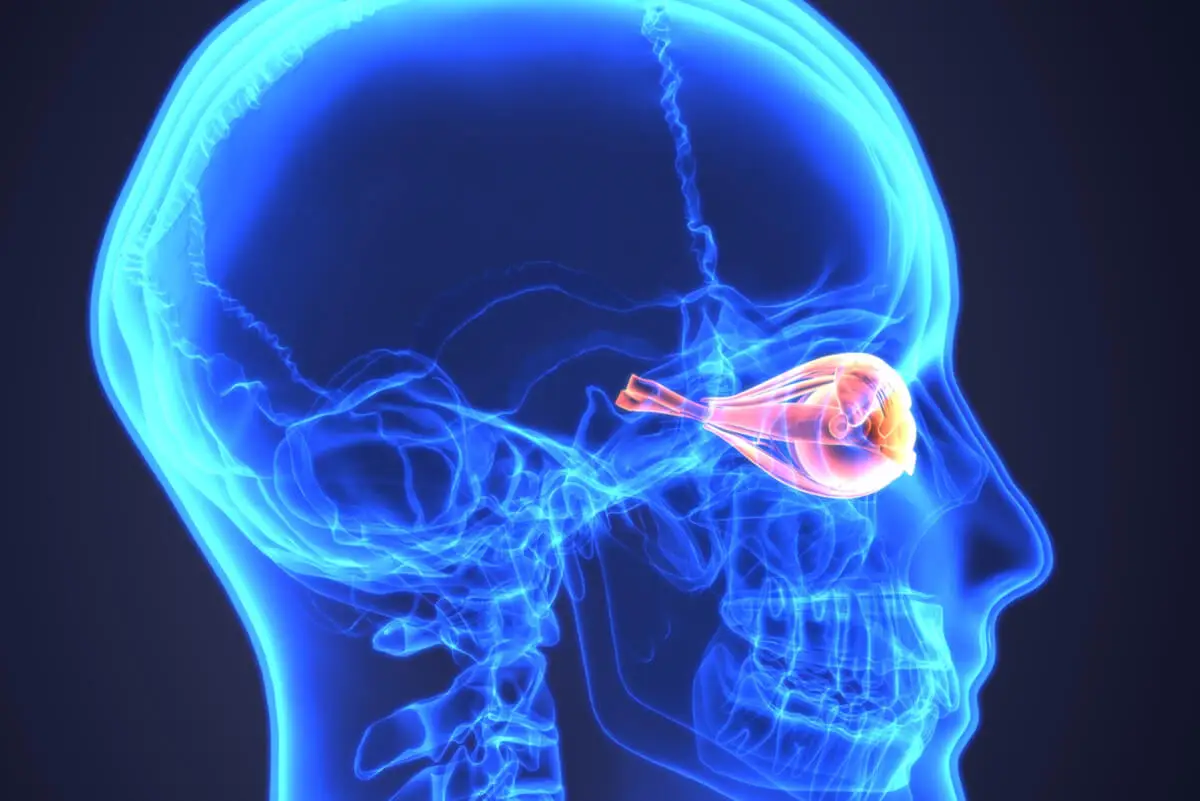
Thyroid eye disease – also known as thyroid ophthalmopathy or thyroid orbitopathy – refers to ocular and periocular changes resulting from thyroid disease. This condition causes an increase in the volume of the extraocular muscles and orbital fat, resulting in proptosis or bulging eyes, colloquially speaking.
Thyroid eye disease has an annual incidence of 16 women and 3 men per 100,000 inhabitants per year. It’s one of the most common anatomical eye diseases, accounting for 70% of orbital conditions.
The basis of thyroid eye disease
Thyroid eye disease is an autoimmune disease. As indicated by the portal NanosWeb (North American Neuro-Ophthalmology Society), the immune system of the patient with this condition produces factors that stimulate the enlargement of the muscles that move the eye.
Four of the facial muscles are the most affected. These include the superior rectus, lateral rectus, inferior rectus, and medial rectus.
All of these muscles originate at the back of the ocular apparatus – at the back of the orbit – and attach to the eye behind the cornea. In normal situations, they’re not directly visible.
For reasons that will be discussed later, the patient’s immune system attacks fibroblasts. These are cell types of connective tissue that synthesize fibers – collagen and glycosaminoglycans – and maintain the extracellular matrix of tissues.
When the immune system damages fibroblasts, widespread inflammation of the eye muscles occurs. With their enlargement, the eyeball pushes forward, resulting in proptosis. Difficulty in closing the eyes and protrusion of the blood capillaries lead to generalized redness.
We think you may also like to read this article: Presbyopia or Eyestrain
What are the symptoms?
The Institute of Ocular Microsurgery (IMO) shows us the most common symptoms of this condition. Thyroid eye disease manifests with orbital inflammation in the form of swelling of the eyelids, protrusion of the eyeball, eyelid retraction, and, sometimes, strabismus.
Once the condition has started, the period of inflammation can last up to 2 years. In addition, in the most severe cases, vision is compromised in around 5% of patients.
Some of the most common clinical signs are the following:
- Foreign body sensation in the ocular apparatus, irritation, and tearing due to corneal exposure.
- Double vision due to strabismus.
- Decreased visual acuity, which happens due to optic nerve compression.
The manifestation is usually bilateral – i.e., in both eyes -, but sometimes there is a clear asymmetry in the progression between one eye and the other. In addition to all the clinical signs described, the patient may manifest photophobia and intense pain in the retrobulbar area.

Why does it occur?
Although it seems like a simple clinical entity, giving an answer to this question is a task that is still under development. The Journal of Endocrinology and Nutrition tells us that everything points to the cause of thyroid eye disease being autoimmune for 3 reasons:
- Some immune abnormality at the level of the thyroid gland is found in all patients. From 25% to 50% of people with Graves’ hyperthyroidism present with manifestations of ophthalmopathy.
- Many patients respond well to the administration of immunosuppressants.
- There’s usually a proximity in time between the onset of hyperthyroidism and thyroid eye disease.
The most widely accepted hypothesis is that the immune system recognizes some antigens – substances that activate antibodies – common between thyroid and orbital tissues. Although the antigen responsible for this response has not yet been identified, sources already cited indicate that it is the TSH (thyrotropin hormone) receptor.
Thyroid eye disease and hyperthyroidism
As mentioned above, the antibodies involved in ophthalmopathy are the same as in hyperthyroidism. Specifically, they are TRAb or TSI, also known as anti-TSH receptor antibodies. Fibroblasts of the orbital musculature present these receptors.
Up to 50% of patients with Graves hyperthyroidism will eventually develop this ophthalmopathy. Other signs that accompany ocular involvement, due to thyroid malfunction, are nervousness, fatigue, muscle weakness, weight loss, sleep problems, and tremors.
How is it diagnosed?
The Clínica Universidad Navarra (CUN) shows us the protocol that should be followed to quantify ocular involvement in the patient. The most common methods include the following:
- First of all, the professional must verify that there’s no corneal involvement. It’s therefore necessary to rule out clinical entities such as keratitis.
- A CT (computed tomography) and MRI (magnetic resonance imaging) can help to elucidate how inflamed the eye muscles are.
- These imaging methods will also help to assess the level of optic nerve involvement. It’s very important to detect if this clinical sign is present, as it causes partial or total loss of vision.
- Depending on the degree of eye involvement, a professional can perform visual acuity, visual field, and color vision tests.
In any case, the diagnosis is multidisciplinary, as it requires the evaluation of an ophthalmologist and an endocrinologist alike. TSH, T3, and T4 testing and thyroid antibody blood tests will help to detect the presence of this problem at a systemic level.
The treatment of thyroid eye disease
In general, thyroid eye disease has a positive prognosis. Estimates indicate that up to 2/3 of patients spontaneously improve, 22% remain stable and only 13.5% worsen. Moreover, in most cases the ophthalmopathy is mild.
General treatment of mild cases
When it’s mild, patients are recommended to use eye protection (glasses), artificial tears during the day, and eye lubricants at night, as indicated by the Endocs portal. In addition, a doctor may also indicate raising the head of the bed to sleep in an upright position.
Endocrinological control
Antithyroid drugs and beta-blockers help to reduce the hyperproduction of thyroid hormones and the symptoms associated with hyperthyroidism. They may also use active iodine therapy and, in the most severe cases, surgery to remove part or most of the thyroid gland.
Corticosteroid pulses
The patient takes high doses of corticosteroids intravenously. This approach lasts for about 6 weeks and is only for cases of optic nerve impingement.
Surgical treatments for proptosis
There’s a surgical procedure to correct the protrusion of the eyeball. Some of the medical approaches for this clinical sign are as follows:
- Orbital decompression: This is used to treat severe exophthalmos, a surgeon can increase the space of the orbital cavity (bony decompression) and reduce its fat content (fat decompression).
- Correction of eyelid retraction: For this purpose, the muscles responsible for eyelid elevation weaken.
- Strabismus surgery: This is focused on correcting double vision caused by exophthalmia.
You may be interested in: 19 Common Eyelid Disorders and their Treatment
Thyroid eye disease is treatable
As you may have noticed, thyroid eye disease is a common clinical entity in people suffering from hyperthyroidism. In spite of alarming clinical signs at an aesthetic level, only 3-5% of cases are severe, and some go away on their own.
As a final note, it’s necessary to highlight that scientific sources emphasize that smoking increases the likelihood of severe forms of this disease. That’s why quitting smoking is a necessity so that the disease does not progress.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- Enfermedad ocular tiroidea, NanosWeb. Recogido a 4 de marzo en http://www.nanosweb.org/files/public/Spanish_ThyroidEyeDisease.pdf
- ¿Qué es la orbitopatía tiroidea? IMO. Recogido a 4 de marzo en https://www.imo.es/es/orbitopatia-tiroidea
- Sánchez-Covisa, M. A. (2006). Tratamiento de la oftalmopatía tiroidea. Endocrinología y Nutrición, 53(9), 550-558.
- Afectación ocular por el hipertiroidismo, CUN. Recogido a 4 de marzo en https://www.cun.es/enfermedades-tratamientos/enfermedades/afectacion-ocular-hipertiroidismo
- Oftalmopatía tiroidea, endocs. Recogido a 4 de marzo en http://www.endocrino.cat/es/tiroides.cfm/ID/6187/ESP/oftalmopatia-tiroidea.htm
- El cigarrillo y la enfermedad ocular tiroidea, intramed. Recogido a 4 de marzo en https://www.intramed.net/contenidover.asp?contenidoid=52548
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








