The Different Types of Mastitis and Their Characteristics

There are different types of mastitis. However, regardless of the type, it’s usually a painful and frustrating experience for mothers breastfeeding their children. It’s actually one of the main reasons why women stop feeding their children this way.
The most worrying part of this is that both the mother and the baby suffer the effects of mastitis. The mother suffers from a psychological and health point of view, and the child because mastitis may lead to a higher risk of death. As such, it’s a problem that we should pay attention to, especially in serious cases.
In this article, we’ll explain what the characteristics are for each type of mastitis and how you can treat it.
What is mastitis?
There are several definitions for mastitis. In the majority of them, the words inflammation and infection of the mammary glands are used.
This is a condition that usually affects women that are breastfeeding. However, there’s also a form of mastitis that occurs in those that aren’t.
Treatment, therefore, depends on the cause. Typically, this infection is due to milk retention. Maternal milk contains substances that, if kept for a prolonged amount of time in the mammary gland, can lead to inflammation and infection.
The rate of developing this condition is relatively high: about 10% of all women that breastfeed suffer from mastitis. Furthermore, although it’s almost always present in just one breast, it can be present in both. Generally speaking, it typically occurs in the first three months after the baby is born, between the second and the third week.

Mastitis usually occurs when breast feeding due to infections.
You may also like: Breast Pain and the Menstrual Cycle
Types of mastitis
As we’ve already mentioned in this article, there are several types of mastitis. The most common types are typical, subacute/subclinical, and recurrent. There are also other less frequent types like tuberculous and granulomatosa.
Typical mastitis
Typically, mastitis is characterized by the full development of infection. As such, it presents a clinical picture with several characteristic symptoms. Among these symptoms we can observe the following:
- Fever up to 102-104°F with eventual chills
- Lack of energy and joint pain
- Swelling or bloating in the affected area
- Pain to the touch on the nipple and the rest of the breast
- Visible reddening
- Heat sensation
- Enlarged skin around the areola
- Lumps under the skin
- Wounds on the nipple
- Irritation and cracking of the nipple and areola
The treatment for typical mastitis depends on the specifics of the infection and symptoms. In this sense, specialists usually recommend a course of 7 to 10 days. They may also recommend the use of analgesics, anti-inflammatory, or antipyretic agents.
Next, let’s take a look at the different types of mastitis.
Keep reading: 5 Reasons for Breast Pain
Types of mastitis: Subacute/subclinical mastitis
- Pain: Moderate to intense
- There may be cramps or sharp pains
- No external symptoms like reddening of the skin, other than a visible tightening
- It may be diagnosed by a laboratory culture exam
- As part of its treatment, it’s recommended to consume probiotics. Furthermore, the person should massage and stretch the pectoral zone.
Recurring mastitis
- This refers to the occurrence of various episodes of mastitis during breastfeeding the same child
- It can happen due to late, inadequate, or insufficient treatment
- Also, it can be caused because of a lack of proper breastfeeding technique
- On occasion, underlying issues like cysts or tumors can cause it
- Another possible cause is a yeast infection (candida albicans)
- For this type, specialists typically prescribe those affected antibiotics and analgesics for the pain
Types of mastitis: Mastitis in women who aren’t breastfeeding
- This is also known as periductal mastitis. Its cause is unknown, but it is more common in women who breastfed for a short time.
- It’s also linked to menopause and may present itself in women between the ages of 45 and 55 years
- It usually just affects just the nipple but can affect the whole breast
- Symptoms range from inflammation, irritation, and reddening, to localized heat, pain, itchiness, and the presence of lumps
- It’s detected by a sonograph
- Professionals proscribe the individual affected with antibiotics, anti-inflammatories, painkillers, and creams
- Certain cases may require surgery
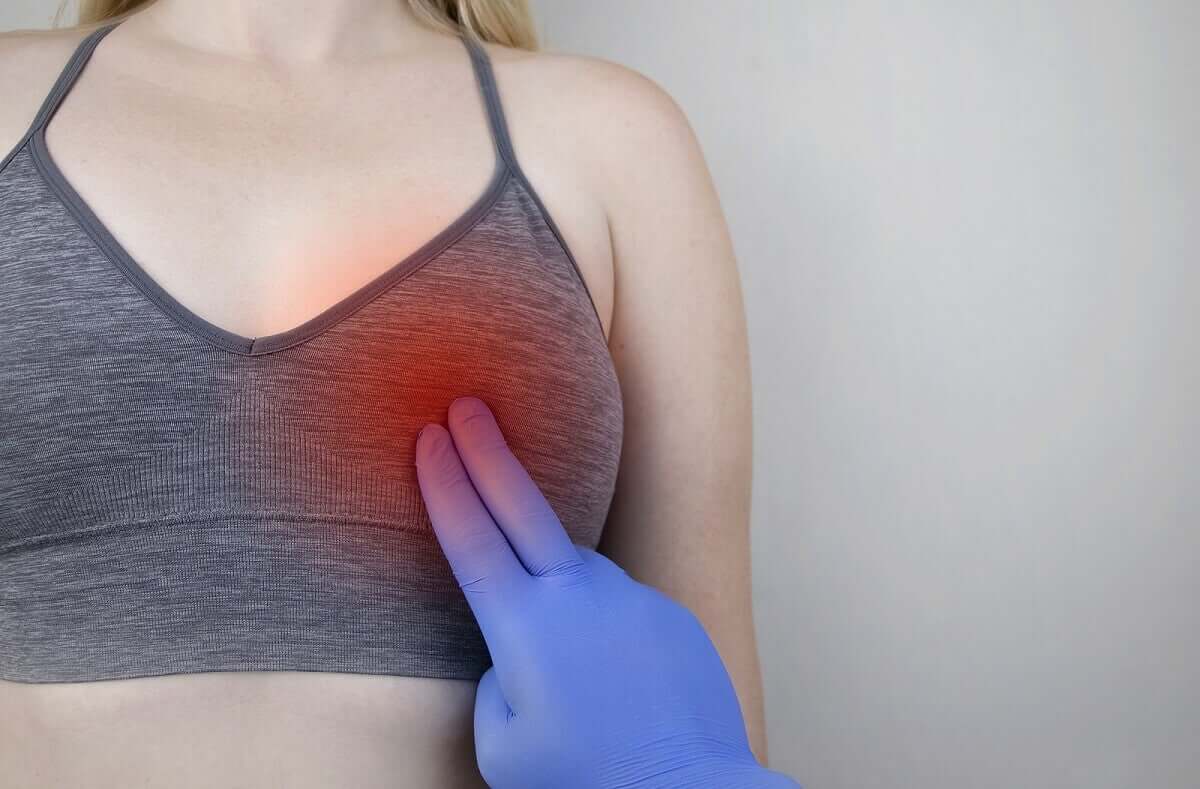
Not all types of mastitis occur as a result of breast feeding. In fact, in some women, it develops after reaching menopause.
What to do if you think you may be developing mastitis
If a woman is breastfeeding and suspects she may have mastitis, she should visit a medical professional. However, this doesn’t mean that she should stop breastfeeding. On the contrary, breastfeeding can have a positive effect. If necessary, the woman can also extract the milk using some kind of device.
Here are some other general recommendations that are good to follow:
- Maintain good posture when breastfeeding
- Massage the chest
- Don’t wear tight-fitting bras
Not treating mastitis in time or adequately can lead to complications. For example, if a milk duct is blocked and there’s an accumulation of pus in the breast, it may need to be medically drained. If that is the case, you should seek medical attention immediately.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- Asociación Española de Pediatría. Manual de lactancia materna. De la teoría a la práctica, Madrid: Editorial Médica Panamericana, 2009.
- Cárdenas N. Estudio de las propiedades tecnológicas de bacterias aisladas de leche materna: aplicación para el desarrollo de alimentos funcionales [Tesis doctoral]. Madrid: Universidad Complutense, 2015. Disponible en: https://eprints.ucm.es/33549/1/T36524.pdf
- Departamento de Salud y Desarrollo del Niño y del Adolescente de la OMS. Mastitis: causas y manejo. Ginebra: Organización Mundial de la Salud, 2009. Disponible en: http://whqlibdoc.who.int/hq/2000/WHO_FCH_CAH_00.13_spa.pdf
- Martínez A, Galbe J, Esparza M. Cuando amamantar duele. Revista de Pediatría y Atención Primaria. 2017; 26: 101-109. Disponible en: http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S1139-76322017000300015
- Paricio J. Diagnóstico y manejo de la mastitis en la madre lactante. En: ponencia presentada en el IX Congreso Español de Lactancia Materna. Zaragoza: Asociación Española de Pediatría, 2017. Disponible en: http://www.e-lactancia.org/media/papers/Mastitis_Texto-CongrLM_Zar-Paricio.pdf
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








