Blood When Coughing or Spitting: When to Seek Help


Written and verified by the doctor Maryel Alvarado Nieto
Blood leaving through the mouth when coughing or spitting can generate a visual impact on people, which in many cases forces them to seek early medical consultation. There are many different causes of this symptom, and they can vary from trivial and easy to handle problems to true emergencies. That’s why blood when coughing or spitting should be carefully evaluated.
The priority is to differentiate the origin of the blood, as it can come from the respiratory tract or even the gastrointestinal tract. This requires a thorough medical questioning followed by a thorough physical examination to recognize the findings in each case.
In addition, being able to show evidence of the blood is a very useful additional resource, since it’s possible for doctors to observe distinctive features, such as the presence of air bubbles or food debris.
Hemoptysis: Blood from the lower airway
The outflow of blood through the mouth that accompanies coughing is known as hemoptysis. The blood that comes out this way often has a frothy appearance, without any food debris.
It’s important to determine the intensity of hemoptysis. To do this, the volume of bleeding and the speed at which it develops must be assessed.
The severity can be classified as follows:
- Mild, known as hemoptotic expectoration. In these cases, blood appears in the form of streaks that stain the sputum.
- Moderate, constituting moderately severe hemoptysis.
- Threatening, which indicates a severe condition in which active bleeding compromises the patient’s breathing or hemodynamic stability.
The causes of blood when coughing or spitting
There are several causes of hemoptysis, which vary in frequency in different geographic populations. Also, age, smoking, and social status are important factors in the search for the source of coughing blood.
The main causes of hemoptysis include the following:
- Bronchiectasis
- Bronchogenic carcinoma
- Chronic bronchitis
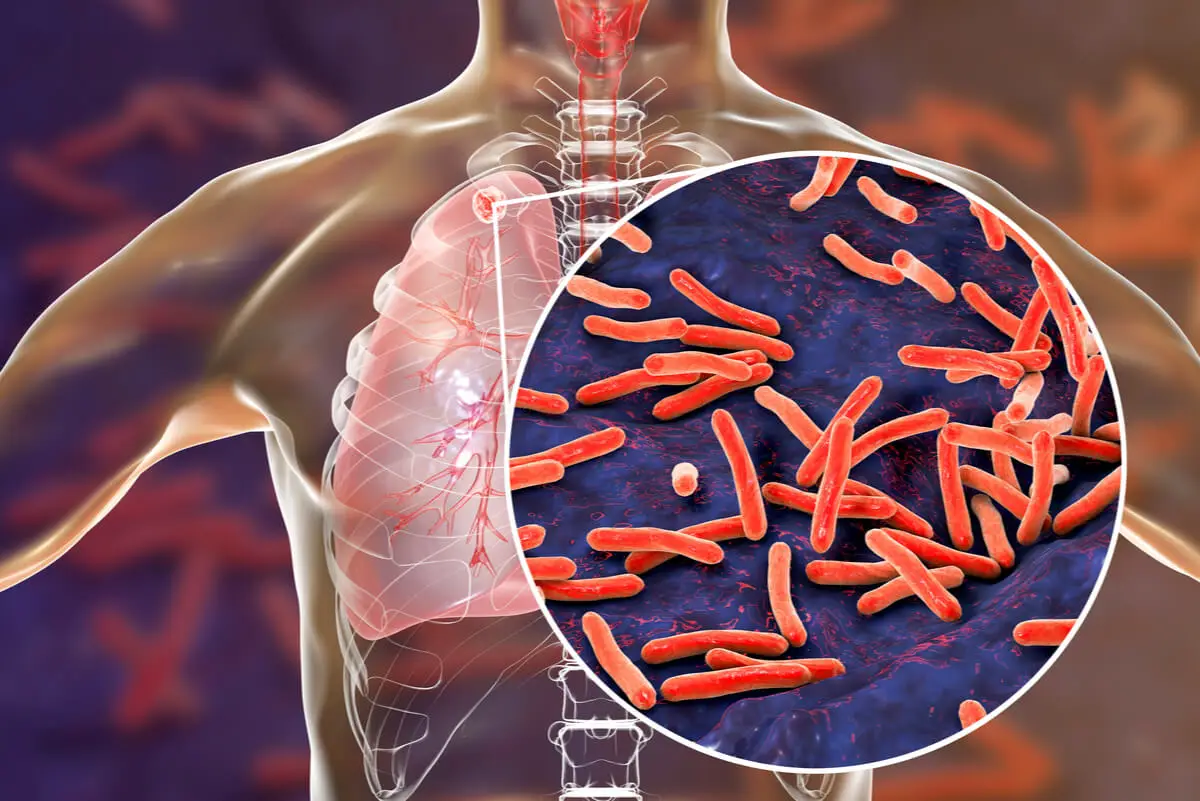
- Tuberculosis
- Pulmonary infections and abscesses
- Mycosis: aspergillosis, histoplasmosis, paracoccidiomycosis, coccidiomycosis
- Thoracic trauma
- Foreign body in the airway
- Arterial malformations
- Use of anticoagulant drugs
- Cryptogenic hemoptysis: cases without an apparent cause
Diagnosis of hemoptysis
A detailed history is helpful in guiding the diagnosis. However, it’s also necessary to perform complementary studies to define the cause and establish an effective treatment.
These tests will depend on each case:
- Hemogram and blood coagulation tests
- A pulse oximetry
- Arterial gas
- An electrocardiogram and cocardiogram
- A sputum study
- A chest X-ray or chest tomography.
- A bronchoscopy
We think you may be interested in reading this, too: Bleeding Hemorrhoids: How do You Treat Them?
Treatment of hemoptysis
The therapeutic approach to coughing up blood depends on the severity of the clinical picture. In mild hemoptysis, outpatient treatment with monitoring at 24 to 48 hours is the most indicated.
In more severe cases, hospitalization is necessary with a controlled diet to prevent bronchoaspiration of food. Antitussive medications and bed rest may in lateral decubitus position on the side of the affected lung may also be indicated in these cases.
Similarly, the airway should be protected, thus ensuring oxygen supply. The use of antibiotics is indicated in the case of a suspected infection and as a prophylactic measure for certain conditions.
The effectiveness of tranexamic acid or aminocaproic acid in stopping bleeding is still not fully understood by doctors.
Other treatment options include therapeutic bronchoscopy, embolization of pathological arteries, and surgery. In addition, globular concentrates should be available for possible transfusion.
Blood from the digestive tract: Hematemesis
Outflow of blood from the mouth accompanying vomiting is known as hematemesis and is a common cause of emergency department consultation. The sites of origin of upper gastrointestinal bleeding (UGH) are the esophagus, stomach, and the duodenum.
Upper gastrointestinal bleeding is classified as either variceal and non-variceal disease, the latter being the most common. Non-varicose causes include the following:
- Esophagitis
- Gastric and duodenal ulcers
- Mallory Weiss syndrome
Like this article? You may also like to read: Dark or Cloudy Urine: 11 Possible Causes and Their Treatment
Risk factors for HDA
Doctors can determine the origin of bleeding by questioning, but this should be verified by an upper GI endoscopy. Even so, there are conditions that predispose to digestive mucosal injury and subsequent bleeding.
Risk factors for upper gastrointestinal bleeding include the following:
- Taking medication with non-steroidal anti-inflammatory analgesics (NSAIDs)
- A history of gastroesophageal reflux
- Helicobacter pylori infection.
- The use of anticoagulant agents and antiplatelet drugs.
- A recent history of profuse vomiting
- Alcoholism
Management and complications of hematemesis
A detailed clinical history is always very useful when it comes to diagnosing and treating hematemesis. Similarly, the intensity of the bleeding should be estimated by paying attention to the hemodynamic conditions of the patient.
Several studies advise the administration of intravenous fluids and the indication of proton pump inhibitors. The possibility of blood transfusion should also be evaluated.
An early endoscopy is currently considered to be the technique of choice, since it makes it possible to determine both the site of the lesion and its severity. This is also sometimes used as a therapeutic technique.
The main complications of upper gastrointestinal bleeding are the risk of rebleeding and perforation of a hollow viscus. Therefore, doctors should examine each case individually while taking into account the person’s age and other existing conditions.

Epistaxis and gingivorrhage: Common causes of blood on coughing or spitting
In addition, injuries to the nose and oropharynx should also be ruled out. Epistaxis, which is bleeding through the nose, and gingivorrhage, which occurs through the gums, are also part of the differential diagnosis.
These are common causes of blood coming out when coughing or spitting. Examination of the nasal passages will reveal the stigmata of the bleeding, while observation of the oral mucosa will allow visualization of areas of inflammation in the gums.
This evaluation is essential, because when epistaxis or gingivorrhage occurs during sleep, it may go unnoticed by the person. This creates confusion, because the next morning blood appears when coughing or spitting and it seems to have no known origin.
When to seek medical help
Whenever bleeding is abundant, it’s essential to go to the nearest emergency room. Likewise, when the presence of blood when coughing or spitting is habitual, it’s necessary to seek a timely medical evaluation.
This is especially the case when the blood clearly doesn’t come from the gums or nose. However, if epistaxis and gingivorrhage bleeding is something you commonly experience, it’s also important to see a doctor.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- Argente, H.; Álvarez, M.; Semiología Médica. Fisiopatología, Semiotecnia y Propedéutica. Enseñanza Basada en el Paciente; Editorial Panamericana;
- Cordovilla, R.; Bollo, E.; Núñez, A.; Cosano, F.; Herráez, I.; Jiménez, R.; Diagnóstico y Tratamiento de la Hemoptisis; Archivos de Bronconeumología; Sociedad Española de Neumología y Cirugía Torácica; 2016.
- Haro, M.; Vizcaya, M.; Jiménez, J.; Tornero, A.; Etiología de la Hemoptisis: Análisis Prospectivo de 752 Casos; Rev Clín sp; 201: 696 – 700; 2001.
- Echeverría, S.; González, W.; Polanco, D.; Ramírez, J.; Vargas, K.; Sangrado Digestivo Alto: Una Emergencia Médica; Revista Ciencia y Salud: Integrando Conocimientos; 4 (4); 2020.
- Aguayo, O.; Torres, A.; Sosa, K.; Ramírez, A.; Rodríguez, C.; Fernández, A.; Bordón, A.; Causas de Hemorragia Digestiva Alta no Varicosa; Cir. Parag.; 37 (1); 2013.
- Martínez, J.; Garrido, A.; Martínez, N.; Pinós, P.; Gil, I.; García, A.; Actuación ante una Epistaxis; Medicina Integral; 35 (7); 2000.
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








