Yellow Vaginal Discharge: 5 Causes and Treatment

Reviewed and approved by the doctor Diego Pereira
Vaginal discharge is a naturally occurring mixture of vaginal secretions and cervical mucus. To a lesser or greater extent, every healthy woman produces it. Its color and odor vary from case to case, although it’s generally considered normal. However, some episodes, such as yellow vaginal discharge, may indicate an underlying condition.
It all depends on the characteristics of the discharge. Before the menstrual period, some women are likely to have a yellowish discharge, as hormonal changes affect its composition. However, if it’s the first time you have it, you should never overlook it. Today we’ll tell you everything you need to know about yellow vaginal discharge.
Causes of yellow vaginal discharge
As we have already explained, vaginal discharge undergoes alterations in color and odor due to hormonal changes. Among other things, a vaginal discharge helps to prevent infection, lubricate the area during sexual intercourse, and keep the vagina clean.
Under normal conditions, the discharge is light in color, has no odor and can vary in viscosity. Likewise, the amount secreted varies in intensity due to many factors (use of contraceptives, for example). The change is natural, so it isn’t always cause for alarm.
When there is no history of changes in color, it’s likely to be a symptom of an underlying condition. If the discharge is pale yellow, has no odor, and is not accompanied by other signs, it should not be a cause for concern. If there is a change in odor and you develop other symptoms it may be due to the following.
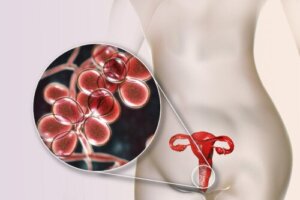
1. Candida spp. infection
Vaginal candidiasis is a fungal infection caused by the fungus Candida albicans (yeast). According to researchers, up to 90% of all vaginal infections are caused by this microorganism. It is so common that Harvard Health estimates that 75% of women will have at least one episode in their lifetime.
Read more about the topic here: 5 Home Remedies to Control Excess Vaginal Discharge and Odors
Symptoms include changes in the color of the vaginal discharge. Although the discharge often takes on a pale white color, it can also acquire a yellowish tone. It usually has no odor, or an odor with a very low intensity.
This alteration of the vaginal discharge is also accompanied by itching and burning in the vagina, discomfort when urinating, pain or discomfort during sexual intercourse, inflammation of the vulva and redness. Most cases are mild and last from a couple of days to two weeks.
2. Pelvic inflammatory disease

Pelvic inflammatory disease (PID) is a condition characterized by inflammation of the endometrium, fallopian tubes, or peritoneum. It happens, in general, when microorganisms from the vagina ascend and follow their path through the uterus. Bacterial causes, then, explain most cases.
You may be interested in: Types of Vaginal Odor: Causes and Treatment
The Office on Women’s Health reports that up to 5% of Americans have PID. In this condition, the altered color of the vaginal discharge is accompanied by a foul odor, one that can become very intense. Other symptoms include the following:
- Pain when urinating
- Pain in the lower abdomen
- Fever
- Irregular menstrual periods
- Discomfort during sexual intercourse
- Abnormal uterine bleeding
This condition is easily treatable and should be treated as soon as possible to avoid complications. For example, it can cause chronic pain, infertility, or problems during pregnancy.
3. Chlamydia
Chlamydia is a sexually transmitted disease (STD) that doesn’t usually cause symptoms. This is why, according to researchers, the percentage of undiagnosed women without symptoms ranges from 1.7% to 17%. Some of the signs you may develop are the following:
- Painful urination
- Abnormal vaginal discharge (in color and odor)
- Pain during sexual intercourse
- Bleeding between menstrual periods
- Fever and nausea (only if the infection has spread)
If the infection isn’t treated in time it can reach your uterus or fallopian tubes. As a consequence, you can develop PID and problems with fertility or during pregnancy. Fortunately, it is treatable and, if done in time, the consequences are practically nil.
4. Trichomoniasis

Although trichomoniasis is one of the most common STDs, most people aren’t familiar with its symptoms. According to studies, this condition is the most common non-viral STD in the world. That’s right: it’s a disease caused by a parasite and not a virus.
In general, the infection doesn’t cause symptoms, although some women may develop the following:
- Yellow, brown, gray, or green vaginal discharge with a foul odor
- Pain during sexual intercourse
- Painful urination
- Redness and burning of the genitals
The infection is easily treated, although it depends on how advanced it is. If not treated in time, it can increase the risk of contracting HIV and lead to infertility problems or complications during pregnancy.
5. Gonorrhoea
Another of today’s common sexually transmitted infections is gonorrhea. According to a Mayo Clinic publication, it is caused by the bacterium Neisseria gonorrhoeae and can affect both men and women. In the latter case, it is characterized by affecting the cervix, so vaginal symptoms are common:
- An increased amount of discharge, which may become yellowish (with or without odor)
- Small amounts of bleeding unrelated to menstruation
- Occasional pelvic pain
- Burning during urination, especially when the urethra is involved
Several risk factors increase the chances of developing this condition, which is common in many conditions of this type. Two of these are having unprotected sex or multiple sexual partners.
Can yellow vaginal discharge be prevented?
Because there are so many different conditions that can cause yellow vaginal discharge, it is important to keep in mind that there’s no single universal measure to prevent it. However, a combination of all these practices could help a great deal:
- Taking care of intimate hygiene by avoiding the use of douches and sprays, as they alter the normal bacterial flora and pH
- Using condoms, especially with new partners
- Avoiding other risky activities that increase the risk of STDs, such as promiscuity
- Not wearing tight trousers or underwear, as it’s always necessary to ventilate the area. In addition, underwear should preferably be made of cotton.
Treatment for yellow vaginal discharge
The conditions we have brought you are just a selection of some of the causes of yellow vaginal discharge. In general, most cases are due to an infectious process, one that can be easily treated with antibiotics or antifungals. Topical creams can also be used to alleviate the symptoms.
However, it’s best to see a specialist for an accurate diagnosis. For example, the use of antibiotics is useless against a fungal infection, while antifungals will not help stop an infectious process caused by parasites or viruses.
The specialist will also determine the extent of the damage, in order to rule out, or confirm, possible problems in your reproductive system. It will also give you the peace of mind of knowing that the treatment is in the hands of a professional. If you think that the yellow vaginal discharge is a symptom of something more serious, don’t hesitate to consult an expert.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- Aduloju, O. P., Akintayo, A. A., & Aduloju, T. (2019). Prevalence of bacterial vaginosis in pregnancy in a tertiary health institution, south western Nigeria. Pan African Medical Journal, 33(1). https://www.ajol.info/index.php/pamj/article/view/208339
- Curry, A., Williams, T., & Penny, M. (2019). Pelvic inflammatory disease: diagnosis, management, and prevention. American family physician, 100(6), 357-364. https://www.aafp.org/pubs/afp/issues/2019/0915/p357.html
- Gazal, L., Terraciano, P., Wolf, N., Dos Santos, F., de Almeida, I., & Pandolfi, E. (2022). The correlation between Chlamydia trachomatis and female infertility: a systematic review. Revista Brasileira de Ginecologia e Obstetrícia/RBGO Gynecology and Obstetrics, 44(06), 614-620. https://www.thieme-connect.com/products/ejournals/html/10.1055/s-0042-1748023
- Kissinger, P. (2015). Trichomonas vaginalis: a review of epidemiologic, clinical and treatment issues. BMC Infectious Diseases, 15, 1-8. https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-015-1055-0
- Mohseni, M., Sung, S., & Takov, V. (2019). Chlamydia. StatPearls Publishing: Treasure Island https://europepmc.org/article/nbk/nbk537286
- Nieto, J., Dávila, F., Intriago, A., & Campusano, J. (2021). Diagnóstico y tratamiento de la gonorrea. Reciamuc, 5(1), 78-89. https://www.reciamuc.com/index.php/RECIAMUC/article/view/595
- Reekie, J., Donovan, B., Guy, R., Hocking, J., Kaldor, J., Mak, D., Preen, D., Ward, J., & Liu, B., (2019). Risk of ectopic pregnancy and tubal infertility following gonorrhea and chlamydia infections. Clinical Infectious Diseases, 69(9), 1621-1623. https://academic.oup.com/cid/article/69/9/1621/5335756?login=false
- Van Gerwen, O., & Muzny, C. (2019). Recent advances in the epidemiology, diagnosis, and management of Trichomonas vaginalis infection. F1000Research, 8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6758837/
- Van Gerwen, O., Craig‐Kuhn, M., Jones, A., Schroeder, J., Deaver, J., Buekens, P., Kissinger, P., & Muzny, C. A. (2021). Trichomoniasis and adverse birth outcomes: a systematic review and meta‐analysis. BJOG: An International Journal of Obstetrics & Gynaecology, 128(12), 1907-1915. https://obgyn.onlinelibrary.wiley.com/doi/abs/10.1111/1471-0528.16774
- Vázquez, F., Fernández, A., & García, B. (2019). Vaginosis. Vaginal microbiota. Enfermedades infecciosas y Microbiología Clínica (English ed.), 37(9), 592-601. https://www.sciencedirect.com/science/article/abs/pii/S2529993X19301698
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








