What Tests Detect a Pericardial Effusion

A pericardial effusion is a condition where there’s an excessive accumulation of fluid between the heart and the pericardium. The latter is the sac that covers the heart. It’s estimated that there’s an effusion when the liquid exceeds 50 ml. So, how can we detect a pericardial effusion?
Between the heart and the pericardium there’s always a thin layer of fluid. However, when you have an illness or injury, it can become inflamed. This, in turn, increases the amount of liquid. Despite this, you can sometimes get a pericardial effusion without prior inflammation.
Pericardial effusion presses on the heart and affects how it works. If left untreated, it could cause heart failure and lead to death. Read this article to learn about the analyses that detect a pericardial effusion.
Ways to detect a pericardial effusion
Echocardiogram
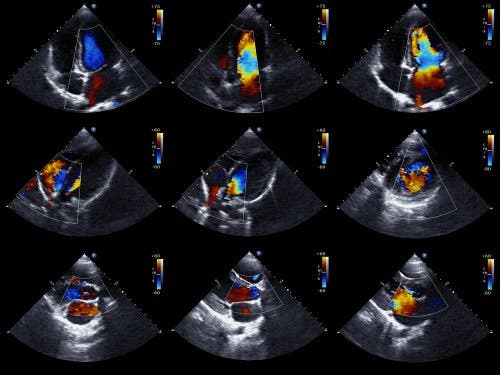
An echocardiogram is the preferred test to detect a pericardial effusion. It’s also called echocardiography or a cardiac ultrasound, and it’s a test that lets doctors see the structure of the heart and study its ability to pump blood.
The Doppler echocardiogram also lets doctors determine the exact speed of the blood flow from the heart. From a technical point of view, the two-dimensional and M-mode echocardiogram is the ideal technique for diagnosing, quantifying, and monitoring pericardial effusion.
Finding an absence of echoes between the epicardium and the lateral pericardium allows doctors to diagnose a pericardial effusion. Then, the cardiologist determines the size of the effusion based on the amount of space between the two layers of the pericardium.
We should note that there are basically two types of echocardiogram. There’s the transthoracic, in which a device is placed on the chest, over the heart, and it emits sound. And the transesophageal, in which the device is inserted into the digestive tract up to the esophagus. The latter provides more detailed data.
Discover: Acute Coronary Syndrome (ACS)
Electrocardiogram
An electrocardiogram records the electrical activity of the heart. Basically, it lets doctors evaluate the rhythm and cardiac function. Pericardial effusion causes alterations in the graph, but they aren’t specific.
Generally, doctors can see certain abnormalities in the QRS complex. This is a vector that reflects the sum of all the electrical discharges that occur in the cells of the ventricles. In general, when there is pericardial effusion, doctors can see a reduction in QRS voltage.
Likewise, in these cases they can observe a flattening of the T waves. If the effusion is very severe and there’s blockage, they can observe an electrical alternation. Typically, the P wave appears wide and bimodal, suggesting an abnormality.
Chest x-ray, CAT scan and MRI

Chest radiography is an X-ray image that allows doctors to see all organs in the chest area. Computed axial tomography, or a CAT scan, is a test that also uses x-rays and allows doctors to get images in the form of cross-sections or in three dimensions.
For its part, magnetic resonance imaging (MRI) is an examination in which doctors get detailed images of the interior of the body, in two or three dimensions. It provides much more specific information than that of the x-ray or the CAT scan.
When there’s pericardial effusion, there’s an alteration in the cardiac silhouette, which one or all of these tests can detect. Usually, the silhouette enlarges when more than 250 ml of fluid accumulates in the pericardial sac.
However, only with more than 50 ml can you talk about pericardial effusion. Therefore, a chest x-ray, for example, doesn’t show the enlarged silhouette, even if the abnormality is present. CAT scans and MRIs are much more conclusive.
Quantification of pericardial effusion
There are no universally accepted criteria for quantifying the volume of the pericardial effusion. This is because all methods have limitations in determining the actual amount of fluid in the pericardial sac.
The most accepted technique for quantification is the one proposed by Weitzman. It’s based on M-mode echocardiography. It proposes adding the echo-free spaces in the anterior and posterior sacs at the end of the diastole. They call it a slight effusion when the sum is 10 mm or less; moderate, between 10 and 19 mm, and severe when it’s 20 mm or more.
It’s important to rule out the presence of cardiac tumors and pericardial cysts, before making the diagnosis. Likewise, doctors should verify that there’s no pleural effusion, or epicardial fat.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- Martín-García, A. C., Peláez, E. D., Martín-García, A., & Sánchez, P. L. (2017). Derrame pericárdico. Taponamiento cardíaco. Medicine-Programa de Formación Médica Continuada Acreditado, 12(44), 2621-2628.
- Sociedad Española de Imagen Cardíaca. Complejo QRS. https://ecocardio.com/documentos/biblioteca-preguntas-basicas/preguntas-al-cardiologo/1046-complejo-qrs.html
- MedlinePlus. Ecocardiografía. https://medlineplus.gov/spanish/ency/article/003869.htm
- MedlinePlus. Trastornos del pericardio. https://medlineplus.gov/spanish/pericardialdisorders.html
- MedlinePlus. Electrocardiograma.https://medlineplus.gov/spanish/pruebas-de-laboratorio/electrocardiograma/
- National Heart, Lung and Blood Institute. Radiografía de tórax. https://www.nhlbi.nih.gov/health-topics/espanol/radiografia-de-torax
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








