Tunnel Vision: What Is It and How to Treat It?


Reviewed and approved by the doctor Leonardo Biolatto
Tunnel vision is a phenomenon in which our ability to perceive certain visual stimuli is affected. With this condition, the perception of elements in the periphery is reduced.
It can be caused by some eye conditions, such as glaucoma, retinitis pigmentosa or retinal detachment; there are also other causes, including psychological ones, as tunnel vision has also been associated with states of stress.
What is tunnel vision?
Sight provides us with information about the elements around us. Generally, we tend to focus on what is directly in front of us. However, if something moves or changes in a nearby location, we will also notice it thanks to peripheral vision.
However, it´s estimated that we can see up to 180° without moving our head. Of these, the central vision picks up only 30°, while the peripheral vision picks up everything else.
This can be altered on certain occasions. For example, when tunnel vision occurs, peripheral perception decreases, fails, or is affected in some way. The sensation described is like looking through a tube.
While there may be no problem focusing on objects in front of you, there is a partial loss of vision, restricting the person’s field of vision. However, some people may not notice it until they close one eye.

Associated symptoms
Tunnel vision is usually more of a sign of certain pathologies. However, there may also be associated symptoms:
- Darkened or diffuse periphery.
- A sensation of vertigo in open spaces.
- The tendency to trip over objects or people.
- The need to turn your head to focus well.
- Difficulty moving around when there are many people.
- Reduced visibility at night or in poorly lit areas, as occurs in patients with astigmatism.
If tunnel vision appears suddenly, the person may experience distress or panic. When it’s gradual, we tend to adapt.
You may also be interested in: Can Stress Affect Your Vision?
Causes of tunnel vision
The phenomenon of tunnel vision can occur due to several causes, both physiological and psychological. Let’s see what they are.
Glaucoma
This is an eye condition characterized by an increase in intraocular pressure. It affects the optic nerve, which sends information to the brain.
According to research, vision loss caused by glaucoma is described as a decrease in peripheral perception.
Retinal detachment
Retinal detachment may be due to trauma or be associated with diseases such as diabetes or arteriosclerosis. Various visual disturbances occur. In addition to tunnel vision, there may be sensations of lights, shadows, a gray spot, flashes like flying flies, among others.
Cerebrovascular accident (CVA)
A stroke can affect the person in various ways, causing hemiplegia (paralysis on one side of the body), hemiparesis (decreased motor control), slurred speech, reduced memory, as well as loss of peripheral vision.
Migraine
Different visual phenomena occur with migraines. For example, so-called auras are mentioned, in which flashes, lights and shapes that aren’t really there are perceived. Also, some people experience tunnel vision temporarily.
Associated psychological factors
Some stress-related disturbances affecting attention and perception have been described. Among these, the phenomenon of tunnel vision can also be found.
It is thought that it may be due to specific hypervigilance, understood as selective attention to certain stimuli, which would be considered by the person as a potential threat, reducing the ability to perceive other elements.
Other causes
There are other possible causes of tunnel vision:
- Optic neuritis
- Brain tumor
- Cranioencephalic trauma
Continue reading: Causes of Poor or Deficient Color Vision
Diagnosis of tunnel vision
There are several causes of tunnel vision. Because of this, you should visit your ophthalmologist if this phenomenon has occurred several times or if it has persisted.
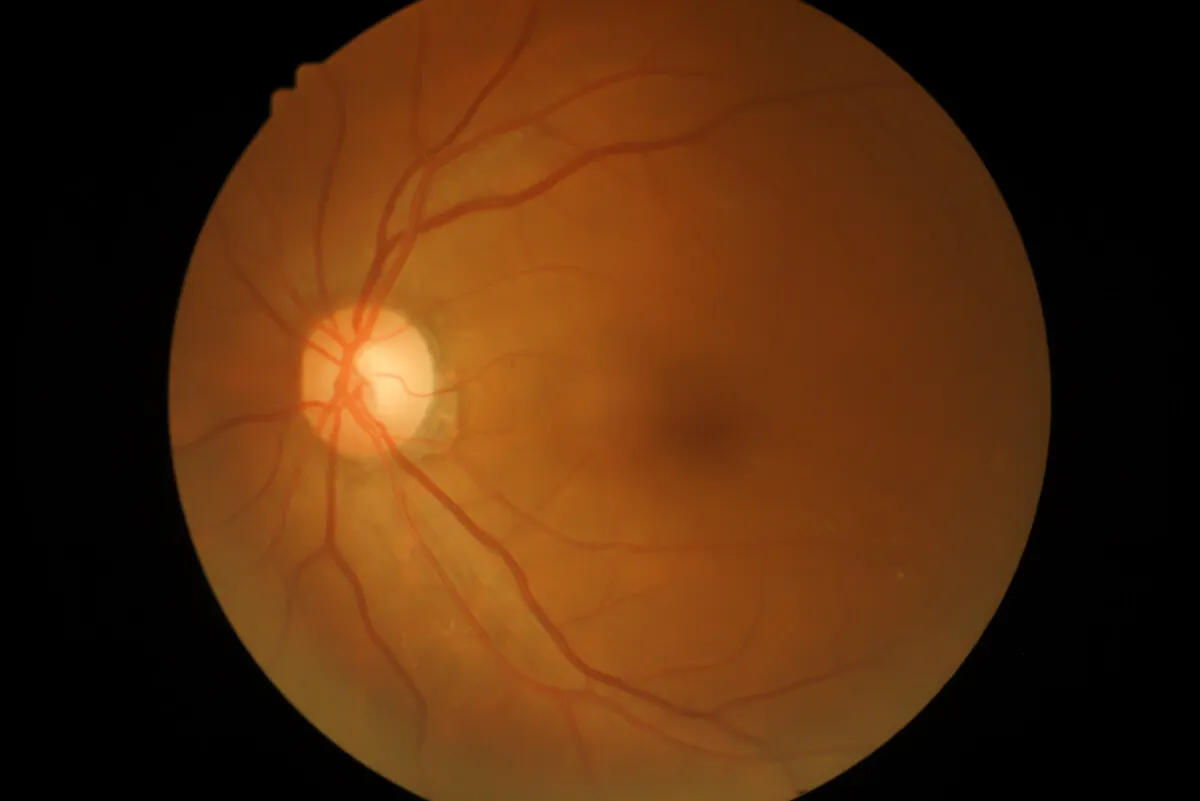
A complete visual examination can help determine the cause. The ophthalmologist will apply drops to dilate the pupils and examine the back of the eye, looking for possible signs of retinal detachment or glaucoma.
Other tests can also be performed to try to establish the cause:
- Ultrasound to visualize the retina
- Optical coherence tomography (OCT)
- Visual field test to measure side vision
- Tonometry to measure the internal pressure in the eye
Treatment options
In relation to treatment, there are several options, but it will depend on each individual cause. In this regard, the following options are available:
- When linked to a stroke, it usually improves on its own. However, it’s important to address the possible causes of the stroke so that it doesn’t recur.
- If tunnel vision is caused by migraines, it’s usually temporary. However, it may occur frequently, so the physician will recommend medication to reduce its recurrence, such as analgesics, dihydroergotamine, and CGRP antagonists.
- In retinal tears, treatments include laser (photocoagulation) or freezing (cryopexy). For detachment, the option is surgery.
- For retinopathy, treatments are being investigated. In this regard, one type of medication used is voretigene neparvovec-rzyl, which, when injected into the eye, can help to treat it, when this condition is caused by the RPE65 gene.
- If tunnel vision is related to glaucoma, eye drops are applied and eventually surgery is performed. In these cases, further damage can be prevented or delayed.
- There’s also the option of vision rehabilitation therapy when tunnel vision becomes permanent.
Can tunnel vision be prevented?
If the symptoms mentioned above are present, it’s important to see an ophthalmologist immediately. And, even though not all cases are reversible, it is possible to avoid further damage which could lead to blindness.
We highly recommend you to have regular eye examinations. While tunnel vision can’t always be prevented, certain possible associated factors can be managed.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- Ayuso T, Aliseda D, Ajuria I, et al. Neuritis óptica inflamatoria. Anales Sis San Navarra. 2009; 32(2): 249-263.
- Castillo M, González P. Estrés y ansiedad. Relación con la cognición. 11vo. Congreso Virtual de Psiquiatria. Interpsiquis. 2010: 1-42.
- Hamel C. Retinitis pigmentosa. Orphanet J Rare Dis. 2006; 40(1): https://doi.org/10.1186/1750-1172-1-40
- Hu C, Zangalli C, Hsieh M, et al. What do patients with glaucoma see? Visual symptoms reported by patients with glaucoma. The American Journal of the Medical Sciences. 2014; 348(5): 403-409.
- Marcos I, Ruiz A, Borrego S, et al. Análisis molecular del gen RPE65 en 72 familias españolas con retinitis pigmentaria autosómica recesiva. Medicina Clínica. 2001;117(4): 121-123.
- Primiani C, Hale D, Shah M, Green K. Clinical Reasoning: a 32-year-old woman with tunnel vision and back pain. Neurology. 2022; DOI: 10.1212/WNL.0000000000201227.
- Santos Lasaosa S, Belvís R, Cuadrado M, et al. CGRP en migraña: de la fisiopatología a la terapéutica Neurología: Publicación oficial de la Sociedad Española de Neurología. 2022; 37(5): 390-402.
- Solís García J, Jordán J. Migraña. Aula de la Farmacia. 2012; 8 (93): 30-38.
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








