Sudden Exanthema: What Is It and How to Treat It?


Written and verified by the doctor Maryel Alvarado Nieto
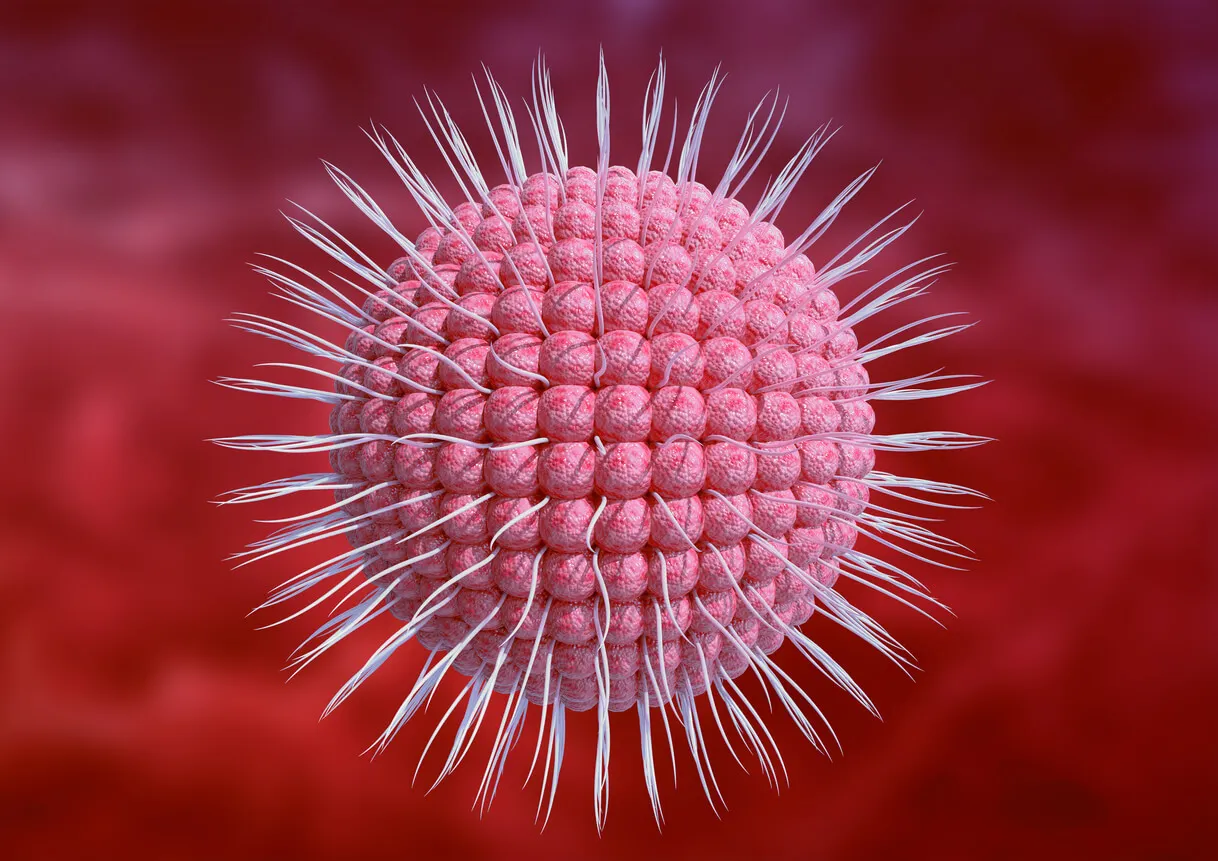
Sudden exanthema, also called infantile roseola, is an infection produced by a virus. At the beginning of the last century, it was part of a group of frequent conditions in children, which had in common the appearance of rashes on the skin.
These conditions, which included measles, rubella and chickenpox, were listed as they were described. In this way, sudden exanthema became known as the “sixth disease”.
The term exanthem refers to the presence of a rash affecting the body surface. When the rash involves the mucous membranes, the term enanthema is used.
Why does sudden exanthema occur?
Sudden exanthema is known to be viral in origin, being caused by human herpes virus (HHV) types 6 and 7. There are two variants of HHV-6 (A and B), but 6B is the one that most frequently produces sudden exanthema.
These viruses are present in more than 95% of adults, and so it’s a highly prevalent infection worldwide.
So far, the mechanism of transmission is believed to be through saliva droplets that are spread by breathing, coughing, or speaking. However, congenital infection is also possible, because HHV has the ability to bind to the genome, transferring with the chromosomes during conception, although this transmission is rare.
The presence of the virus in various cells of the organism is maintained for life.
Who is affected?
More than 95% of those presenting with sudden exanthema are between 6 months and 3 years of age. It is, therefore, considered a typical childhood condition.
However, because the virus remains latent in the body, reactivations are possible, although they tend to go unnoticed. In young infants, this condition is rare because of the protection afforded by maternal antibodies that have crossed the placenta.
Symptoms of sudden exanthema
Sudden exanthema is usually distributed over the chest and abdomen, with minor rashes on the surface of the extremities, the face, and behind the ears. Very occasionally, it’s possible to observe lesions on the palate and uvula.
The initial symptom is fever, which is usually high and lasts for a couple of days. After the temperature normalizes, the typical manifestation appears: a small, irregular, pinkish rash, predominantly on the trunk.
It’s important to note that, because the fever has subsided when the rash appears, the child is usually in good general condition. For this reason, the infection is sometimes underestimated by parents.
In addition to the rash, some patients also have tonsillitis, pharyngitis or otitis media, whose symptoms suggest a viral origin. Similarly, the enlargement of the neck lymph node chains is common, but examining these isn’t painful for the child.
In some patients, the infection may be symptomless. Other less common manifestations include the following:
- Diarrhea
- Vomiting
- Headaches
- Abdominal pain
- Reddish spots on the palate and uvula.
After 24 to 48 hours, the rash completely disappears.
It should be noted that sometimes, because of a fear of the high fever, antibiotics might be prescribed in haste. As the rash appears a few days later, it’s easy to misinterpret it as a drug-sensitivity reaction.
Read more: Antibiotics: Some of the Inherent Risks
Complications of sudden exanthema
It isn’t yet known which patients are most likely to develop complications, but up to one-third of children are at risk. The most serious are those affecting the central nervous system (CNS), including febrile convulsion and encephalitis.
As for the mechanisms capable of producing neurological manifestations, much remains to be discovered. In fact, some authors say that the virus remains in the CNS after the first infection, bringing with it an increased risk of febrile convulsion and neurological symptoms in the patient.
However, there are discrepancies among the different studies, so more research is needed.
On the other hand, although the sudden exanthema is usually considered to be unimportant, people with immune system deficiencies and those who have received transplants show a greater predisposition to more severe infections, as well as a higher risk of complications and the reactivation of the viral process. Therefore, close follow-up of transplant recipients is vital.
How is sudden exanthema diagnosed?
The infection can be diagnosed medically, and this is based both on the presence of the rash and on the remission of the fever before the rash appears. Complementary tests aren’t indispensable, but they can determine the existence of antibodies.
Similarly, polymerase chain reaction (PCR) is used to detect viral DNA. But its cost, when compared to the condition’s relative lack of seriousness, doesn’t justify its regular use.

Differential diagnosis
The main difference with the other exanthematous childhood diseases is that in this condition the fever subsides before the appearance of lesions. On the other hand, the rash’s characteristics help distinguish it from other viral processes.
However, it’s important to know some related diagnoses:
- Chickenpox
- Scarlet fever
- Measles
- Infectious mononucleosis
Find out more here: 5 Types of Common Newborn Rashes
Treatment of sudden exanthema
As it’s a viral process that completely remits spontaneously, it doesn’t need any specific treatment. Therefore, the recommendation is simply to manage the child’s symptoms.
This means that antipyretics should be prescribed to treat fever. Similarly, it’s important to recommend rest and fluid intake.
Some authors consider that the administration of antivirals (ganciclovir, for example) could have some usefulness in reducing the viral load. However, this theory hasn’t been proven and more research is needed.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- Baquedano, I.; Bernadó, R.; Aznar, S.; Bustillo, A.; Guerrero, C.; Encefalofatía por Virus Herpes 6 como Complicación de Exantema Súbito; Archivos Argentinos de Pediatría; 116 (2); 2018.
- Berenberg, W.; La Roséola Infantil o Exantema Súbito; Anales de Medicina y Cirugía; 28 (63): 249 – 253; 1950.
- Berría, M.; Herpes Virus Humano-6: Potencial Neuropatogénico y Asociación Clínica con Enfermedad Neurológica; Medicina; 59 (3): 305 – 308; 1999.
- Compilación: Arteaga, R.; Arteaga, R.; Infecciones por Herpes Virus Humano 6 y 7; Resúmenes de Artículos de la Literatura Pediátrica; Revista de la Sociedad Boliviana de Pediatría; 44 (1): 38 – 40; 2005. Basado en: Ward, K.; Current Opinion in Infectious Diseases; 28; 247 – 252; 2005.
- González, N.; Aguilar, N.; Rivera, E.; Hernández, C.; Infecciones por Herpes Virus Humano Tipo 7 en Pediatría; Revista Latinoamericana de Infectología Pediátrica; 32 (3): 109 – 102; 2019.
- Palacios, C.; Durán, C.; Orozco, L.; Saéz, M.; García, M.; Ruiz, R.; Exantemas en Pediatría; Acta Pediátrica de México; 36: 412 – 423; 2015.
- Vega, T.; Gil, M.; Rodríguez, M.; de la Serna, P.; Red de Médicos Centinelas de Castilla y León; Incidencia y Características Clínicas de los Exantemas Maculopapulares de Etiología Viral; Atención Primaria; 32 (9): 517 – 523; 2003.
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








