Intracranial Hematoma: What Is It and How Is It Treated?

Written and verified by the doctor Leonardo Biolatto
An intracranial hematoma is often life-threatening. And, although many others may be small, its evolution must be monitored. It’s not a matter to consider lightly, nor to let it pass as just another symptom.
This problem develops when blood accumulates inside the skull bones. The locations of this blood collection are varied, and the clinical picture will change according to those positions.
One of the problems of these hematomas is the pressure they generate on a sensitive organ such as the brain. This increased tension hurts the neurons and complicates their functioning.
The mild form of intracranial hematoma is the one that manifests itself with a concussion, that is, a brief loss of consciousness with complete recovery. However, severe forms can also occur, resulting in the death of the patient.
The accumulation of blood derives from a ruptured blood vessel within the skull. This may be ruptured by trauma or by spontaneous rupture of an artery, in cases of congenital malformations, for example.
Types of intracranial hematomas
According to their location within the skull, there are three types of intracranial hematomas.
Subdural hematoma
The subdural hematoma is located below the dura mater, which is one of the layers of the meninges. In the process, one or more blood vessels are ruptured, bringing the collection of blood to that region, where it’s trapped. If the size is large, there’s a serious risk to life.
When it’s acute, the risk is greater. This is the one that, classically, appears immediately after a traumatism. Symptoms are not long in coming and are usually quite evident, with loss of consciousness, nausea, convulsions and pain.
Another variety is subacute subdural hematoma, which forms progressively, manifesting symptoms within days or weeks. And finally, chronic subdural hematoma, which can last for months. The latter usually starts imperceptibly and develops silently.

Learn more about: The Difference Between the Brain and the Mind
Epidural hematoma
This intracranial hematoma is located between the dura mater and the skull, in the outermost part of the brain, we could say. It’s the blood collection that’s closest to the outside.
The classic cause is trauma, and the complication is the inward pressure they exert. It’s very common for patients with this variety to go through different stages of loss of consciousness.
Intracerebral hematoma
Also known as intraparenchymal hematoma. It’s located within the brain tissue, in the middle of the neurons, hence its name. It can originate in trauma, but also when strokes happen due to arterial ruptures or the presence of a congenital malformation.
Some brain tumors are also responsible for this clinical picture. Their treatment is more complicated because it involves a difficult position with serious risks of sequelae.
Treatment of intracranial hematoma
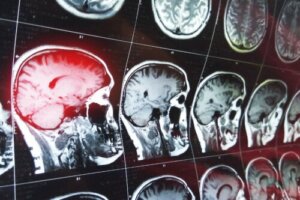
When doctors detect an intracranial hematoma, they establish its size and position. This is accomplished by imaging techniques such as CT or MRI.
If the intracranial hematoma is small, doesn’t exert pressure, and the patient’s symptoms are stable, no specific treatment is recommended. In addition, alarm guidelines are given and the patient is usually monitored again after a period of time.
In larger, life-threatening cases, doctors plan for surgery. There are two approaches: localized drainage or craniotomy. Localized drainage is intended to have the least possible impact on the skull.
For this purpose, a surgeon will make a minimal hole in the skull to insert a probe and drain the blood from the hematoma outwards. In large lesions it isn’t possible to do so, and doctors use a craniotomy with a frank opening of the bones.

What to do if you suspect an intracranial hematoma
If we have had a head injury, or suffer symptoms that make us suspect problems in the brain, the ideal thing would be to consult a doctor immediately. As we’ve just said, these are serious health problems that are life-threatening.
Health professionals will perform complementary methods to determine the presence of an intracranial hematoma, its size and position. Based on this, they can plan surgery, drainage or periodic check-ups.
Patients taking anticoagulant drugs should pay special attention, as they’re an aggravating factor for hematomas that worsen the picture. The physician attending these patients should know from the first moment that the patient is consuming these drugs.
A timely consultation can be life-saving; therefore, it’s essential not to delay care in these cases. In conclusion, an intracranial hematoma is a medical emergency and you should treat it as such.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- Iglesias, Román, et al. “Concausality in a clinical case of subdural hematoma.” Medicina Legal de Costa Rica 34.2 (2017): 113-117.
- Quintana, E. Murias, et al. “Tratamiento combinado, mediante embolización y cirugía, de los aneurismas cerebrales rotos con hematoma cerebral e hipertensión intracraneal: Análisis retrospectivo y revisión de la bibliografía.” Radiología 61.1 (2019): 42-50.
- Ortega Santiesteban, Orlando, et al. “Diagnosing a subdural hematoma: a clinical-imaging dynamic process.” Revista Médica Electrónica 41.2 (2019).
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








