High Levels of Monocytes in the Blood: Symptoms and Treatments
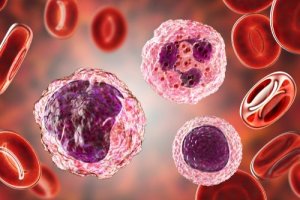
Our blood contains many more cell types and substances than most people typically know. A good example of this is monocytes. Monocytes are immune system cells that circulate in the blood.
The bone marrow produces monocytes, which then reach various tissues through the blood. When they reach the tissues, they become macrophages and perform their defense function. They’re responsible for removing certain waste products and dangerous elements from the body. Moreover, these cells also act in inflammatory processes.
Overall, monocytes represent between 4 and 8% of the total cells in the blood. However, their concentration varies depending on age, infections, or if there’s an active inflammatory process.
In this article, we’ll explain why you may have high levels of monocytes in your blood. This is an essential factor to be taken into account during a blood test or when it comes to knowing a person’s immune status.
Why do blood monocyte levels elevate?
As we mentioned above, monocytes are cells that belong to the immune system. They’re key players in inflammatory and infectious processes. Medical professionals consider their levels high when their amount exceeds 8% of all blood cells.
High levels of monocytes in the blood don’t have to cause symptoms. However, what usually do manifest are the symptoms and signs of the situation that’s causing this increase. In short, we can say that the most common causes are:
- Infections. The truth is that infections are the most common cause, even if they’re transient infections.
- Autoimmune and inflammatory diseases. The most common of these is rheumatoid arthritis.
- Blood disorders.
- Carcinogenic processes, such as leukemia and lymphoma.

You may like this article: A Simple Blood Test Could Locate Tumors
High levels of monocytes due to infection
This is the most common cause. Monocyte levels elevate both due to a simple infection, such as a cold, as well as a chronic infection, like tuberculosis. However, blood tests that show high levels of monocytes are non-specific.
Inflammatory diseases
These cells may also be an indication that there’s an inflammatory process in the body. This is the case of rheumatoid arthritis. It’s a chronic inflammatory disorder that affects the joints and causes pain and loss of mobility.
Blood neoplasms
The blood cells may also experience neoplastic processes. This means that different types of cells can grow uncontrollably and increase their concentration. Thus, this may also be a cause of high levels of monocytes in the blood.
This article may interest you: A Blood Test to Diagnose Depression
How doctors detect high levels of monocytes in the blood
Blood tests that include a complete blood count show all the cells present in the blood. This is a simple and effective method to detect this situation. However, as we indicated above, some data are nonspecific and should be studied more deeply.
Depending on the number of monocytes, it’s more likely that it’s due to a process or another. For example, if the levels are slightly elevated, it’s probably due to a mild infection. On the other hand, if the levels are excessively high, they may be indicative of leukemia.
The doctor will be responsible for analyzing the concentration of monocytes. As they deem necessary, they may request other tests to find the infection or inflammatory process, if they exist. Therefore, it’s very important to know if the patient has other symptoms that accompany this fact. There’s no treatment for high blood monocytes. Instead, the treatment is focused on solving the underlying cause.
Nevertheless, we should also emphasize that exercise can be a way to improve your monocyte count. This is because exercise helps regulate immune system functioning and acts as a natural anti-inflammatory.
In conclusion, it’s important to remember that high levels of monocytes is a very nonspecific sign. You need to see your doctor to get diagnosed. In addition, most of the time, it’s a consequence of a mild passing infection.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- Abarca, A. (2016). Ejercicio como tratamiento anti-inflamatorio. Medicina Legal de Costa Rica, 33(1), 228-233. Disponible en: https://www.scielo.sa.cr/scielo.php?script=sci_abstract&pid=S1409-00152016000100228&lng=en
- de la Calle-Fabregat, C., Rodríguez-Ubreva, J., Ciudad, L., Ramírez, J., Celis, R., Azuaga, A. B., Cuervo, A., Graell, E., Pérez-García, C., Díaz-Torné, C., Salvador, G., Gómez-Puerta, J. A., Haro, I., Sanmartí, R., Cañete, J. D., & Ballestar, E. (2022). The synovial and blood monocyte DNA methylomes mirror prognosis, evolution, and treatment in early arthritis. JCI Insight, 7(9). Disponible en: https://doi.org/10.1172/jci.insight.158783
- García-Casal, M., & Pons-Garcia, H. (2014). Dieta e inflamación. Anales Venezolanos de Nutrición, 27(1), 47-56. Disponible en: http://ve.scielo.org/scielo.php?script=sci_arttext&pid=S0798-07522014000100009&lng=es&tlng=es.
- García Díaz, M. F., Iglesias Fernández, N., Menéndez Ordás, R. E., Pardo Vega, R., García González, V., & Sánchez Fontecha, M. C. (2014). Utilidad de la serie blanca en el diagnóstico diferencial de la mononucleosis infecciosa. Pediatría Atención Primaria, 16(64), e127-e131. Recuperado de: https://dx.doi.org/10.4321/S1139-76322014000500002
- Hirose, S., Lin, Q., Ohtsuji, M., Nishimura, H., & Verbeek, J. S. (2019). Monocyte subsets involved in the development of systemic lupus erythematosus and rheumatoid arthritis. International immunology, 31(11), 687–696. Recuperado de: https://doi.org/10.1093/intimm/dxz036
- Huerta Aragonés, J., Cela de Julián, E. (2018). Hematología práctica: interpretación del hemograma y de las pruebas de coagulación. En: AEPap (ed.). Curso de Actualización Pediatría 2018. Madrid: Lúa Ediciones 3.0, 507-526. Recuperado de: https://www.aepap.org/sites/default/files/507-526_hematologia_practica.pdf
- Jordan, S., Tung, N., Casanova-Acebes, M., Chang, C., Cantoni, C., Zhang, D., Wirtz, T. H., Naik, S., Rose, S. A., Brocker, C. N., Gainullina, A., Hornburg, D., Horng, S., Maier, B. B., Cravedi, P., LeRoith, D., Gonzalez, F. J., Meissner, F., Ochando, J., Rahman, A., … Merad, M. (2019). Dietary Intake Regulates the Circulating Inflammatory Monocyte Pool. Cell, 178(5), 1102–1114.e17. Disponible en: https://doi.org/10.1016/j.cell.2019.07.050
- León, B., López-Bravo, M., & Ardavín, C. (2005). Monocyte-derived dendritic cells. Seminars in immunology, 17(4), 313–318. Recuperado de: https://doi.org/10.1016/j.smim.2005.05.013
- Mangaonkar, A. A., Tande, A. J., & Bekele, D. I. (2021). Differential Diagnosis and Workup of Monocytosis: A Systematic Approach to a Common Hematologic Finding. Current hematologic malignancy reports, 16(3), 267–275. Recuperado de: https://doi.org/10.1007/s11899-021-00618-4
- Ochoa-Carrillo, F. J. (2013). Los macrófagos, ángeles o demonios. Gaceta Mexicana de Oncología, 12(1), 1-3. Disponible en: https://www.elsevier.es/es-revista-gaceta-mexicana-oncologia-305-articulo-los-macrofagos-angeles-o-demonios-X1665920113933087
- Pinto, T., Rossoni, A., Rodrigues, C., Rossoni, M., & Tahan, T. (2017). Diagnosis of tuberculosis in children: the role of hemogram and inflammatory markers. Residência Pediátrica, 7(Supl), 17-19. Disponible en: https://doi.org/10.25060/residpediatr-2017.v7s1-05
- ¿Qué significan los Monocitos altos? | ClinicPoint. (n.d.). Retrieved January 5, 2020. Recuperado de: https://www.clinicpoint.com/blog/316/que-son-monocitos-altos
- Territo, M. (2020). Trastornos de los Monocitos. Manual MSD. Consultado en: https://www.msdmanuals.com/es-es/hogar/trastornos-de-la-sangre/trastornos-de-los-gl%C3%B3bulos-blancos-leucocitos/trastornos-de-los-monocitos
- Torrens, M. (2015). INTERPRETACIÓN CLÍNICA DEL HEMOGRAMA. Revista Médica Clínica Las Condes, 26(6), 713-725. Recuperado de: https://doi.org/10.1016/j.rmclc.2015.11.001
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








