What Is Marchiafava-Bignami Disease? Symptoms, Causes and Treatments

Reviewed and approved by the doctor Mariel Mendoza
Marchiafava-Bignami disease is a rare pathology, in which erosion of the corpus callosum occurs. It occurs most frequently in men with alcohol use disorder, but also in people with severe malnutrition.
Symptoms may include seizures, slurred speech, depression, apathy, and aggressiveness. Treatment includes intravenous or oral administration of thiamine, folic acid, and vitamin B, as well as corticosteroids.
What is Marchiafava-Bignami disease?
This pathology owes its name to the Italian physicians Ettore Marchiafava and Amico Bignami, who described it in 1903. In addition, these pathologists are recognized for having studied and identified the parasite that transmits malaria.
Marchiafava-Bignami disease (abbreviated MBD) is rare. A 2001 study reports a total of 250 reported cases, from men of various nationalities.
Many of them with alcohol use disorder.
It is characterized by demyelination, as well as eventual necrosis, of the corpus callosum. What does this mean? The corpus callosum is a structure located in the brain that connects the two hemispheres, helping both to work in a coordinated manner.
Myelin is an insulating layer, composed of protein and fats. It functions as a sheath, covering and insulating nerves. In addition to this function, myelin contributes to the transmission of electrical impulses.
Symptoms of Marchiafava-Bignami disease
The onset and degree of symptoms of Marchiafava-Bignami disease vary from case to case, depending on whether it’s acute, subacute, or chronic. Some are related to psychological functioning and others are neurological:
- Ataxia
- Apraxia
- Depression
- Dysarthria
- Hemiparesis
- Aggressiveness
- Convulsions
- Visual and auditory hallucinations.
- Spasticity and gait disturbances.
- Confusion, dementia, and paranoia.
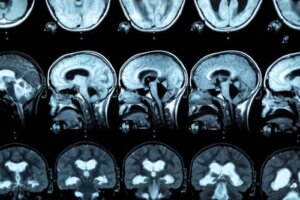
Tumefaction of the corpus callosum can also be appreciated if a cerebral image is made. In some cases, signs of interhemispheric disconnection syndrome are present.
Another great article: 10 Pillars for Your Brain Health
Causes and risk factors
MBD is more common in patients with alcohol use disorder. However, its etiology isn’t entirely clear, as it also occurs in people who don’t have a drinking addiction.
Some research indicates that it may occur in patients suffering from chronic malnutrition. In this regard, it’s thought to be related to a deficiency of B complex vitamins.
Other possible causes mentioned are the following:
- Sickle cell disease and cerebral malaria
- Complication of ketoacidosis in diabetes mellitus
- Malnutrition following gastric-bypass surgery.
- Cardiac carcinoma surgery.
The average age of diagnosed cases is 45 years.
On the other hand, Marchiafava-Bignami disease is more common in men. This is possibly because alcohol consumption is higher in them, according to statistics.
Be sure to visit: 4 Tips to Stop Drinking Alcohol
How is it diagnosed?
For the diagnosis of this pathology, an MRI is performed, so that lesions in the corpus callosum are observed. In this regard, research indicates that people with alcohol use disorder show a reduction in the anterior, middle, and posterior thickness of the corpus callosum, as well as variations in the size of the frontal lobe and cortical sulci.
In addition, the patient’s history is analyzed and detailed physical and psychological examinations are performed:
- Neurological function, using some scales (MOHS and mRS)
- Cognitive function (with tests such as the Montreal or MoCA)
- Alteration of consciousness (Glasgow Coma Scale)
- Alcohol consumption (MAST-C)
General laboratory tests are recommended, such as complete blood count, electrolytes, glucose, transaminases, bilirubin, and cerebrospinal fluid serology panel. The latter is to check for central nervous system infections.
Treatment of Marchiafava-Bignami disease
Treatment for Marchiafava-Bignami disease includes vitamin supplements of thiamine, folate, and other B vitamins. These can be administered intravenously or orally. The dosage varies in each case and will depend on the physician’s indication.
Of course, it’s necessary to stop drinking alcohol. But since this can trigger withdrawal symptoms, additional medication or even hospital admission may be required.

Possible complications
Several studies report that patients with MBD have shown significant improvement after administration of multivitamins and corticosteroids. Although in the case of diabetics, stabilization and normalization of plasma glucose is also required.
However, in the acute stage, damaged areas of the corpus callosum may show cytotoxic edematous changes. There’s also a possibility of lesions in other parts of the brain, such as the cerebral lobes, hemispheric white matter and basal ganglia.
In untreated patients, as well as in those who don’t respond to treatment, demyelination and necrosis may become permanent. Cystic transformation may also occur.
Other damage associated with alcohol or dietary deficiency is not uncommon:
- Abnormal lipid metabolism
- Gastrointestinal disorders
- Metabolic disturbances
- Hypovitaminosis
- Hepatic damage
Also, when the corpus callosum is affected, the connection between both hemispheres fails, resulting in cognitive, sensory and motor problems. Finally, some patients may go into a coma.
Although some may recover spontaneously, others may die. The mortality rate is 20%.
Prognosis
Because the severity of this disease is variable, the prognosis is uncertain. Even with symptoms, a person can survive for years, recover, or, on the contrary, deteriorate until death.
The earlier the diagnosis is made and the more closely treatment is followed, the better the patient’s chances of recovery. This includes cessation of alcohol intake.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- Bachar M, Fatakhov E, Banerjee C, Todnem N. Rapidly resolving nonalcoholic Marchiafava-Bignami disease in the setting of malnourishment after gastric bypass surgery. J Investig Med High Impact Case Rep. 2018; 6: doi.org/10.1177/2324709618784318.
- Boutboul D, Lidove O, Aguilar C, Klein I, Papo T. Marchiafava-Bignami disease complicating SC hemoglobin disease and Plasmodium falciparum infection. Presse Med. 2010; 39(9): 990-993.
- Carrilho P, Santos M, Piasecki L, Jorge A. Marchiafava-Bignami disease: a rare entity with a poor outcome. Rev Bras Ter Intensiva. 2013; 25(1): 68-72.
- Ceylan-Isik A, McBride S, Ren J. Sex difference in alcoholism: who is at a greater risk for development of alcoholic complication? Life Sci. 2010; 87(5-6): 133-138.
- Estruch R, Nicolás J, Salamero M, Aragón C, et al. Atrophy of the corpus callosum in chronic alcoholism. J Neurol Sci. 1997; 146(2): 145-151.
- Helenius J, Tatlisumak T, Soinne L, Valanne L, Kaste M. Marchiafava-Bignami disease: two cases with favourable outcome. Eur J Neurol. 2001; 8(3): 269-272.
- Hillbom M, Saloheimo P, Fujioka S, Wszolek ZK, Juvela S, Leone MA. Diagnosis and management of Marchiafava-Bignami disease: a review of CT/MRI confirmed cases. J Neurol Neurosurg Psychiatry. 2014; 85(2): 168-173.
- Suzuki Y, Oishi M, Ogawa K, Kamei S. A patient with Marchiafava-Bignami disease as a complication of diabetes mellitus treated effectively with corticosteroid. J Clin Neurosci. 2012; 19(5): 761-762.
- Tian T, Pescador M, Park S, et al. Marchiafava Bignami Disease. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022 Jan. Disponible: https://www.ncbi.nlm.nih.gov/books/NBK526007/
- Ventura R. El síndrome de desconexión interhemisférica cerebral. Revista de psiquiatria y salud mental. 2003; IV(2): 29-42.
- Yadala S, Luo J. Marchiafava-Bignami disease in a nonalcoholic diabetic patient. Case Rep Neurol Med. 2013: https://doi.org/10.1155/2013/979383.
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








