Uses and Types of Endotracheal Tubes

Doctors usually insert endotracheal tubes through the mouth or nose. They ensure that the airways are open, and that patients can breathe properly.
Doctors use it under general anesthetic, when a patient is in critical care, needs mechanical ventilation, or got into an emergency with a problem that affects the airways.
Some studies describe this procedure as “invasive mechanical ventilation.” The reason for this is that endotracheal tubes force the airways open. In fact, they do this when they are closed due to the patient’s stress.
In fact, in many situations, it’s necessary to use drugs or some medication to help relax the muscles in the area to allow the endotracheal tubes to go in. Next, we’ll see how doctors use them. In addition, we’ll explain what parts they’re composed of, and what you should take into account.
Parts of endotracheal tubes
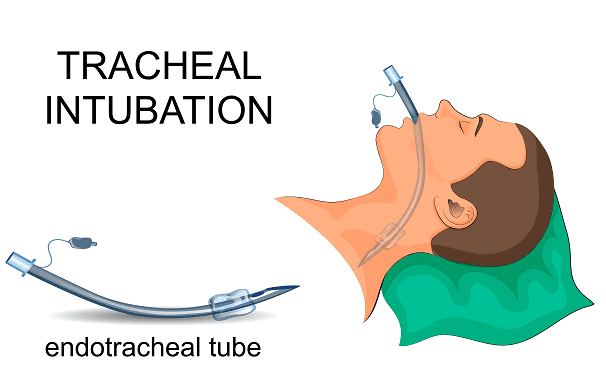
- Connector: This is a piece that connects the tube and respiratory. We could also define it as a mouthpiece, and it’s the opposite part to the one that goes in the airways.
- Body: It’s the main part of the tube that will let oxygen flow through. Normally, it has a light so doctors can see if they’re inserting it properly through the trachea.
- Tip: It’s on the opposite end of the connector, which sometimes has a pointed shape with an orifice called “Murphy’s orifice.” However, not all tubes have this. In fact, it can increase the risk of airway injuries.
- Balloon: It’s close to the connector, and it usually has an adapted and ergonomic design to make it easy to insert. This part of the tube helps reduce pressure on the walls of the trachea. Usually, doctors use it with children.
Types of endotracheal tubes

In addition to the individual parts of endotracheal tubes, there are different types of tubes too. Here are some of them and their characteristics.
- Lumen endotracheal tubes: Sterile devices made with polyvinyl chloride or silicone. Doctors can insert them orally or nasally, and they may need to use anesthesia to make it easier. They have a ball with high volume and low pressure.
- Double lumen endotracheal tubes: Ideal for patients with asymmetric lung disease or who have a bronchopleural fistula. In fact, they allow doctors to get air to just one lung.
- Spacial endotracheal tubes: There are several types, such as laser resistant ones if they’re needed during surgery. Additionally, there’s a spiraling wire reinforcement inside the wall of the tube to prevent the clamping that doctors use in brain and orofacial surgeries.
- Tubes with additional ports: Doctors can administer drugs that patients need in emergencies. For example, they can administer anesthesia or relaxants to help the tube go through the airway.
As you can see, there are different types of endotracheal tubes that can meet patients’ individual needs at a given time. However, let’s see what you need to consider before using endotracheal tubes.
Aspects to take into account
Knowing how to place endotracheal tubes correctly is something that emergency room professionals should know very well. Failure to follow the proper steps and do them incorrectly can put patients’ lives at risk.
First of all, you shouldn’t ever force these tubes into the patients’ throat. If the airways resist because of tension or agitation, you need to give them a calming or relaxing drug so you don’t damage the walls of the trachea.
Also, professionals who perform this type of procedure need to be precise, quick and agile. In addition, they should know what type of tube their patients need so they don’t waste time.
We hope all this information has been useful!
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- Díaz, E., Lorente, L., Valles, J., & Rello, J. (2010). Neumonía asociada a la ventilación mecánica. Medicina intensiva, 34(5), 318-324.
- Ferragut, C. R., & López-Herce, J. (2003, January). Complicaciones de la ventilación mecánica. In Anales de Pediatría (Vol. 59, No. 2, pp. 160-165). Elsevier Doyma.
- Ramón, C. O., & Pablo, Á. A. J. (2011). Manejo avanzado de la vía aérea. Revista Médica Clínica Las Condes, 22(3), 270-279.
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








