New Cancer Treatment? Photoimmunotherapy Successfully Eliminates Malignant Cells

Written and verified by the doctor Leonardo Biolatto
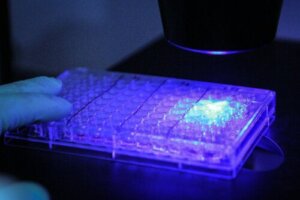
The findings published last month in the journal BMC Medicine are encouraging for those who would like to see a new treatment for cancer. Using a photoimmunotherapy technique, the researchers fluorescently labeled glioblastoma cells and eliminated them in laboratory mice.
With a system that would be doubly useful, as we’ll explain later, the team of scientists is excited to announce that we’re at the beginning of a novel approach to oncological pathologies. Especially for cancer in more dangerous locations or those that tend to return with the passage of time.
The Institute of Cancer Research in London was the institution responsible for the discovery. It was joined by the Imperial College in the same city, the University of Silesia (Poland), and a company of Swedish origin (AffibodyAB ®).
What was the research about?
The scientific study published in May 2022 revealed that the scientists based their research on glioblastoma, specifically in mice. This tumor is malignant and has a rather aggressive behavior, with recurrences over time. It originates from cells called astrocytes.
Human patients with this pathology are difficult to treat. The brain localization makes resection surgeries difficult and limits radiotherapy applications, for example.
What the researchers achieved was to improve the localization of the cancer cells to make surgery easier and with fewer errors. At the same time, the protein combination that serves to mark these malignant cells is capable of being activated later to eliminate any remaining tumor remnants.

Discover more here: Immunotherapy for Cancer: What You Need to Know
How did they reach the results?
Specifically, the research followed the following steps:
- A laboratory protein called affibody was developed. It has a high affinity for cancer cells. That is, it has the ability to bind almost exclusively to tumors and not to other parts of the body. Why? Because it combines with another protein called EGFR, which is characteristic of glioblastoma, for example, and other cancers.
- The antibodies were combined, before being inoculated into the mice, with a molecule called IR700. This substance is fluorescent and can glow with certain techniques to indicate where it is present.
- Mice suffering from glioblastoma were given the combination of the amphibole with IR700. This protein combination bound to the cancer cells.
- Surgeries were performed on the mice, taking advantage of the fluorescence of the apherb/IR700 complex, so surgeons could see more clearly which areas to operate on and which to leave untouched.
- After the surgery was completed, the apherb/IR700 complex was stimulated with near-infrared light. This has the property of activating an antitumor property of the epicures. Thus, this laboratory protein eliminates any cancer cells that may have remained after removal.
Photoimmunotherapies could help attack cancer cells that cannot be removed during surgery, which may help people live longer after treatment.
Is photoimmunotherapy a new treatment for cancer?
To think that we already have a new treatment for cancer is getting ahead of ourselves. The researchers themselves acknowledged in some interviews that there are still technical issues to be resolved. In addition, the tests were carried out on animals.
In any case, it’s worthwhile to be hopeful in the right measure. Neoplasms that are difficult to access, such as those that develop in the brain, have few resources that can treat them.
Surgical limitations in certain parts of the body and the dangers inherent to radiotherapy that damages nearby structures, mean that patients have to adhere to a less successful protocol. Not to mention that the surgery, when performed, have a high risk of leaving sequelae in the nervous system.
Read more here: What Is a Glioma Tumor?
What are the current treatments for neoplasms?
Photoimmunotherapy could be a new treatment for cancer because it would be added to the 4 traditional and classic ways of dealing with malignant tumors:
- Surgery: This method is the oldest and still the most effective. It can be used in accessible and delimited tumor masses.
- Radiotherapy: High doses of radiation are used to reach the cancerous cells and modify their behavior. They may be killed by causing lethal modifications or their growth may be slowed down. The main adverse effects derive from the action of radiation on the patient’s non-malignant cells.
- Chemotherapy: This modality uses pharmacological substances orally or intravenously to attack malignant cells. As with radiation therapy, a major problem is the inability of most of these drugs to distinguish between malignancy and non-malignant cells.
- Immunotherapy: This is a form of biological therapy. It means that substances produced by living organisms are used. In this case, to treat cancer. The aim is to boost the activity of the immune system so that it succeeds in eliminating cancer cells.
This being the case, photoimmunotherapy appears on the horizon as a new treatment for cancer that could have significant effects. The truth is that, as we have made clear, there’s still a long way to go.
However, this recent study, which had the greatest media coverage, isn’t the only one of its kind. There are records of the successful use of near-infrared light in the recent past. Among some relevant examples, we can mention the communication by Isobe and collaborators in 2020, which remitted a small cell lung cancer in mice, as well as the finding by Kiss and his team, who inhibited tumor growth in bladder cancer.
Caution when talking about cancer
Postulating a new treatment for cancer through photoimmunotherapy is a palpable reality. There are several research teams looking for concrete results that demonstrate effectiveness in humans.
But there’s still no such protocol for humans that can be applied to any cancer patient. Therefore, caution should reign.
If you have symptoms that make you suspect cancer or you are already diagnosed, follow the instructions of your oncologist. He/she is the only one qualified to guide you in treating your problem.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- Mączyńska, Justyna, et al. “Triggering anti-GBM immune response with EGFR-mediated photoimmunotherapy.” BMC medicine 20.1 (2022): 1-17.
- Kato, Takuya, et al. “Near infrared photoimmunotherapy; a review of targets for cancer therapy.” Cancers 13.11 (2021): 2535.
- Isobe, Yoshitaka, et al. “Near infrared photoimmunotherapy targeting DLL3 for small cell lung cancer.” EBioMedicine 52 (2020): 102632.
- Kiss, Bernhard, et al. “CD47-Targeted Near-Infrared Photoimmunotherapy for Human Bladder CancerCD47-Targeted Photoimmunotherapy for Bladder Cancer.” Clinical Cancer Research 25.12 (2019): 3561-3571.
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








