Naegleria Fowleri Infection: The Brain-eating Amoeba


Written and verified by the biologist Samuel Antonio Sánchez Amador
Infection with Naegleria fowleri (an amoeboflagellate belonging to the phylum Percolozoa) triggers naegleriasis, also known as primary amebic meningoencephalitis (PAM). This condition is extremely rare and lethal, with a reported mortality rate of 98.5% in patients suffering from it.
Fortunately, this infection is very rare. Only 34 cases have been cited in the United States from 2008 to 2017. Globally, about 450 cases of naegleriasis have been detected in the last 60 years.
N. fowleri lives in freshwater, soil, or within the host’s central nervous system (CNS), with all that entails. If you want to learn more about primary amebic meningoencephalitis, including symptoms and treatments, just keep reading.
What is a Naegleria fowleri infection?
Naegleria fowleri, also known in the general media as the brain-eating amoeba, is a species of the genus Naegleria, belonging to the phylum Percolozoa. It’s not a true amoeba at the phylogenetic level, since it goes through a flagellated life cycle phase, which isn’t the case in the phylum Amoebozoa.
N. fowleri has a special predilection for freshwater environments, especially those that are dirty and contaminated by a substrate. As indicated by the medical portal Statpearls, this organism can withstand temperatures up to 45 degrees Celsius, and its life cycle is divided into three distinct phases:
- Cyst: This is the resistance structure of the microorganism. When the free forms are subjected to stressful environments, they become encysted with a diameter of about 9 micrometers. Factors that promote encystation are lack of food, environmental desiccation, and temperatures below 10 degrees Celsius.
- Trophozoite: This is the stage that divides, feeds on bacteria, and, unfortunately, causes the disease in humans. Trophozoites measure 10 to 35 micrometers and move using pseudopods, cytoplasmic prolongations that allow basic locomotion.
- Flagellated: This stage distinguishes Naegleria from many other non-bacterial microorganisms. The flagellated form, as its name suggests, has 2 flagella and arises when the trophozoites are exposed to ionic changes in the aqueous medium.
You should know that both the flagellate and the cyst can cause infection in humans, although the trophozoite is the infective form per se. When this amoeboflagellate enters the nasal cavity of the host, both forms transform into the infective trophozoite without problems.
Learn about: This Is What Happens to Your Brain When You Don’t Rest
Why does infection occur?
The Centers for Disease Control and Prevention (CDC) shows us the infective cycle of this pathogen. N. fowleri enters the human body through the nasal passages, either as a flagellate, cyst, or trophozoite. Once nasal inoculation has occurred, the pathogen invades the respiratory epithelium and olfactory mucosa.
From here, it migrates through the lamina cribrosa (a section of the ethmoid bone) into the central nervous system (CNS), more specifically into the brain, via the olfactory nerves. The basal aspect of the cerebrum, the cerebellum, and the olfactory bulbs are the most damaged structures in infected patients.
N. fowleri elicits an innate response from the immune system. Its virulence depends on the Nfa1 protein (which binds oxygen molecules), nitrogen oxide production, and the presence of pore-forming proteins.
Since there are no bacteria to feed on inside the human being, N. fowleri preys on neurons and astrocytes of the central nervous system. To some extent, the name brain-eating amoeba honors its pathogenic mechanism.
Risk factors
The Mayo Clinic and other sources indicate the risk factors that are conducive to the development of Naegleria infection. In any case, you should keep in mind that this is a very rare disease:
- Swimming in unsanitized freshwater: Most people become infected after swimming in stagnant water or water present in unsanitized natural environments.
- Swimming in very warm water: This pathogen doesn’t respond well to cold. Therefore, it’s more common in temperate climates.
- Being young: Because of their habits and tendency to reduced hygiene, young children are more prone to N. fowleri infection.
Lastly, you should note that the amoeba doesn’t survive in saline environments and is sensitive to chlorine. It’s impossible to become infected by swimming in the sea or a properly treated public swimming pool.
Symptoms of Naegleria fowleri infection
The clinical signs of infection occur in a range of 2 to 8 days, although some patients begin to feel symptoms after 24 hours, as indicated by the Antimicrobial Agents and Chemotherapy portal. Even so, we must point out that there isn’t a standardized picture.
The most common symptoms are severe headache, photophobia, confusion, epileptic seizures, and coma. Patients have also been observed with abnormal heart rhythms and characteristic necrosis of the myocardium, the muscle tissue of the heart.
In addition to all this, doctors believe the main cause is an increase in intracranial pressure. The pressure in the cerebrospinal fluid increases to 600 millimeters of water in patients with naegleriasis. As mentioned above, the prognosis is very poor and most cases end in death.
Diagnostic tests
As indicated in the MSD Manuals, this disease can only be confirmed by lumbar puncture (and subsequent cerebrospinal fluid analysis), as well as by brain biopsy. Doctors perform these tests on people with symptoms of naegleriasis who have been in contact with untreated fresh water in the last few days.
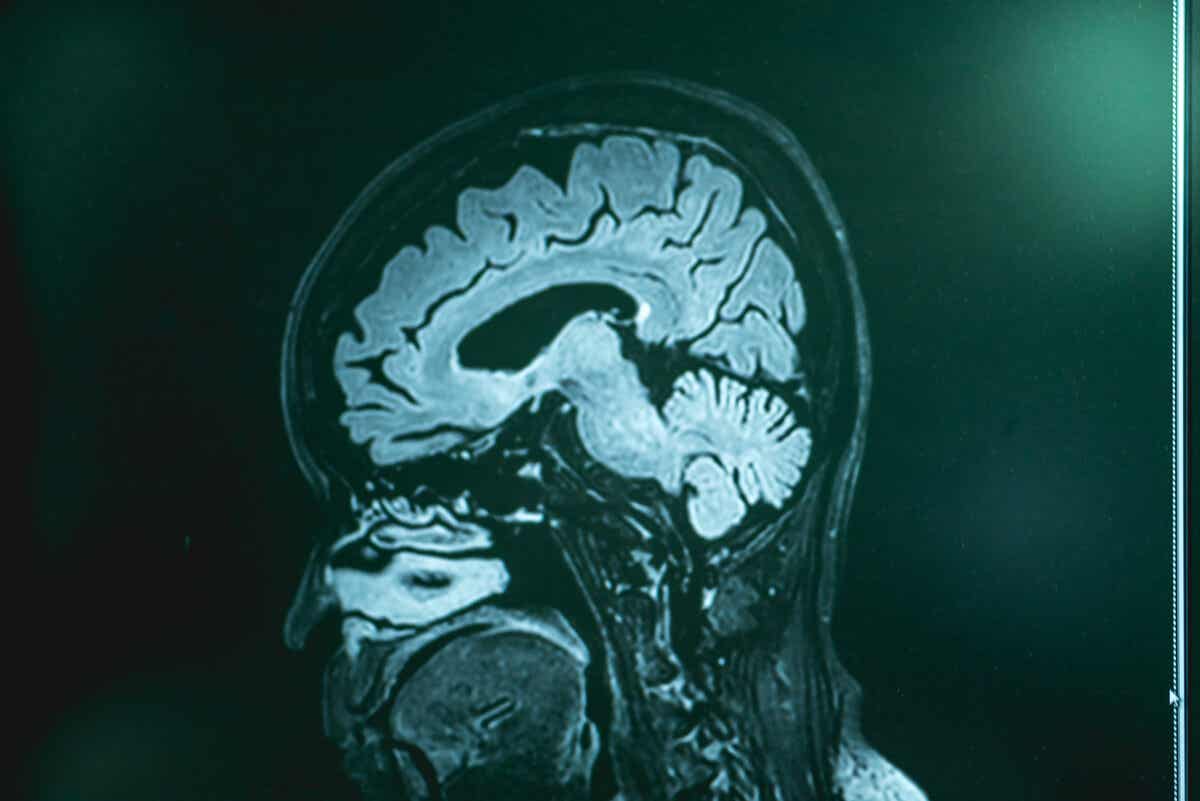
On the other hand, imaging tests (computed tomography and magnetic resonance imaging) don’t detect the disease but can rule out other possible health issues. Once the cerebrospinal fluid has been obtained, doctors perform cultures or genetic analyses in search of the amoeba genome.

Possible treatments for Naegleria infection
Treatment options for Naegleria infection are very limited, due to the lack of surviving patients and in vitro studies conducted.
The following are drugs that are currently in use or are in the trial period, but don’t guarantee a patient’s recovery:
- Amphotericin B: This is an antibiotic and antifungal extracted from Streptomyces nodosus, a filamentous bacterium. It’s the most common medication historically to treat naegleriasis.
- Miltefosine: This is an antiprotozoal agent that was first developed to treat breast cancer. This treatment saved the lives of 3 patients: 2 in 2013 and 1 in 2016.
- Fluconazole: This is an adjuvant drug in the prevention of superficial and systemic fungal infections. It has a good penetration rate into the central nervous system.
- Azithromycin: This is a broad-spectrum antibiotic of the macrolide group. It’s in the experimental stage for this disease.
Unfortunately, there have only been three survivors in the United States in the last 10 years. This makes it very difficult to test the effectiveness of a treatment. Of the nearly 150 people infected in this country in the last 60 years, only 4 have survived to tell the tale.
Also read: Intestinal Bacteria: A Possible Basis For Obesity Treatments
A rare issue you shouldn’t worry about
These latest data may seem alarming, but nothing could be further from the truth. Specialists have detected a total of 148 cases of naegleriasis in the United States in the last 60 years, when 328 million people live in this country today. The disease is so rare and the percentage of people it affects is so small that it isn’t worth worrying about.
Therefore, despite the social alarm that some sources try to sustain, we emphasize that there’s nothing to worry about.
It’s always a good idea to avoid practicing water sports in stagnant waters, because of the possible pathogens that may inhabit them, but beyond this prevention, there’s little else that can be done to avoid infection by Naegleria.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- Pervin, N., & Sundareshan, V. (2020). Naegleria. StatPearls [Internet].
- Naegleria Fowleri, pathogenesis and infection, CDC. Recogido a 6 de abril en https://www.cdc.gov/parasites/naegleria/pathogen.html
- Infección por Naegleria, Mayoclinic. Recogido a 6 de abril en https://www.mayoclinic.org/es-es/diseases-conditions/naegleria-infection/symptoms-causes/syc-20375470
- Grace, E., Asbill, S., & Virga, K. (2015). Naegleria fowleri: pathogenesis, diagnosis, and treatment options. Antimicrobial agents and chemotherapy, 59(11), 6677-6681.
- Infección encefálica amebiana: meningoencefalitis amebiana primaria, MSDmanuals. Recogido a 6 de abril en https://www.msdmanuals.com/es-es/hogar/infecciones/infecciones-parasitarias-protozoos-extraintestinales/infecci%C3%B3n-encef%C3%A1lica-amebiana-meningoencefalitis-amebiana-primaria#:~:text=La%20meningoencefalitis%20amebiana%20primaria%20es,de%20ameba%20de%20vida%20libre.
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








