Joint Prostheses Infection: Why Does It Occur?
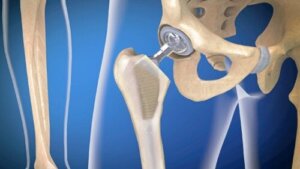
Infection of joint prostheses is a relatively frequent complication following joint replacements. Prosthesis placement is a very widespread surgery nowadays, which helps to treat numerous pathologies related to the bone apparatus.
Most of the cases involve hip or knee prostheses. Although they are procedures with very good results, they can have complications, as with any other surgical technique. Why does this infection occur? What are its symptoms? Below, we’ll answer these questions.
What is joint prosthesis infection?
Joint prosthesis infection is also known as ‘periprosthetic infection’. It’s a complication that compromises both the joint replacement area and the adjacent tissues.
Arthroplasty is the medical name for this procedure. According to information from the Clínica Universidad de Navarra, around 30,000 interventions of this type are performed in Spain every year. This is a safe procedure that, in most cases, produces a notable improvement in the patient’s quality of life.
The joints most likely to be replaced by a prosthesis are the hip and the knee.
Even so, as stated in a publication in Clinical Microbiology Reviews, a minority of patients will experience device failure and require additional surgery at some point in their lives. It’s estimated that 2-4% of arthroplasty cases result in infection.
The big problem is that it can cause other serious complications, as well as high costs to the healthcare system. In itself, it’s usually caused by the patient’s own bacteria, which form a gelatinous matrix on the prosthesis.
What happens is that these microorganisms adhere to the surface of the prosthesis. Once there, they multiply and give rise to this matrix, which is called a biofilm. This is a mechanism that defends them from the action of antibiotics, making them more resistant to treatment.
Why can joint prosthesis infection occur?
Infection of joint prostheses can be caused by different types of bacteria. As we have pointed out, they adhere to the prosthesis and form a biofilm. To do this, they organize themselves in layers, one on top of the other. This explains why those found in the deeper layers are more resistant to antibiotics.
However, the prosthesis itself also alters the function of certain cells of the immune system, such as phagocytes. All these factors favor the progression of the infection and make it difficult to treat.
The bacteria usually involved are staphylococci. Within this group, the most frequent microorganisms are Staphylococcus aureus and Staphylococcus epidermidis. Other agents involved are the following:
- Escherichia coli
- Pseudomonas aeruginosa
- Enterococcus spp
It may also be a polymicrobial infection. That is, it may be caused by more than one bacterium. Fungal infections are less frequent.
We think you may be interested in reading this, too: Joint Hypermobility Syndrome: What Is It and How To Deal With It?
Types of infection
Infection of joint prostheses is usually classified according to the time of evolution. Some authors distinguish between acute and chronic infection. However, as explained in the Prioam Guide, it can also be classified as follows
- Early postoperative infection (PPI)
- Late chronic infection (LCI)
- Acute hematogenous infection (AHI)
Those who only distinguish between acute and chronic infection include acute hematogenous infection in the first group.
Early postsurgical infection or acute infection
Early postsurgical infection is that which occurs in the first month after prosthesis placement. Some consider that it’s still considered acute infection up to three months after surgery.
There are a series of criteria that help to identify this type of joint prosthesis infection. There is usually dehiscence and suppuration of the surgical wound. In addition, when fluid is removed from the joint and examined in the laboratory, the presence of bacteria is often detected.
In these cases, early diagnosis and treatment are important. In this way, the need to replace the prosthesis due to infection can be avoided.
Acute hematogenous infection
Acute hematogenous infection occurs when the focus of infection is elsewhere in the body. In other words, the bacteria can come from another process such as pneumonia, urinary tract infection, endocarditis, etcetera. What happens is that they are mobilized with the blood and end up colonizing the prosthesis.
Infection of an articular prosthesis of chronic type
A chronic infection is usually considered when three months have passed from the placement of the prosthesis. It’s more complicated to treat than acute ones, since the bacterial biofilm has matured and cannot be removed.
This condition evolves progressively and insidiously. Pain persists for months, although there are no clear signs of infection or fever. In some cases, abscesses and fistulas may be present. In these cases, replacement of the prosthesis is usually necessary.
Associated symptoms
The symptoms of joint prosthesis infection vary depending on whether they are acute or chronic. It’s important to note that about half of the cases are chronic. Therefore, one of the predominant symptoms is inflammatory pain.
The problem is that arthroplasties can cause pain without necessarily causing infection. Hence, it’s sometimes difficult to reach a correct diagnosis. In addition to pain, there may be a lack of functionality in the joint.
In cases of acute infection, patients usually present fever. The surgical wound does not heal properly and there may be oozing of purulent material through the wound. The area is usually swollen, warm, and red.
Like this article? You may also like to read: Joint Effusion: What Is It and How Can It Be Treated?
How is joint replacement infection diagnosed?
The diagnosis of this type of infection should be made early. This prevents the infection from becoming chronic and the operation from having to be repeated. In order to do so, it’s important to monitor the patient properly and to be attentive to any warning signs.
However, there are a number of complementary tests that can help in the diagnosis. One of these is positron emission tomography. This is a technique that uses a glucose tracer. This molecule is captured by the bacteria causing the infection.
Thus, by means of the scan, the areas where the bacteria are located can be appreciated. Other useful tests are synovial fluid analysis and blood tests. Ultrasounds and X-rays can also be useful.
Available treatments
Infection of joint replacements requires multidisciplinary treatment. In all types, medical and surgical treatment is usually combined. The medical treatment is based on reducing pain and administering specific antibiotics to cure the infection.
Surgery can be used to clean and debride the tissues. In cases where the infection is chronic, prosthesis replacement is likely to be required. This can be done as a one-stage or two-stage procedure.
That is, the new prosthesis can be placed in the same surgery. The two-stage option involves removing the prosthesis, cleaning the area, and placing a spacer containing antibiotics. Then, in another operation, the new prosthesis is placed.
In order to establish antibiotic treatment, it’s recommended to first identify the causative germ and its sensitivity to these drugs. The duration of treatment can be long. In some cases, such as knee prostheses, six months of treatment may be recommended.
Remember: An infection of joint prostheses can be serious
Although this isn’t a very common complication, an infection of prostheses is very feared by surgeons. This is because in some cases it requires further surgery and replacement of the prosthesis.
It’s important for patients to be aware of the signs and symptoms in order to be able to identify an infection early. In addition, physicians should make the diagnosis as quickly as possible, as this reduces the likelihood of needing to operate again.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
-
Ayoade F, Li DD, Mabrouk A, et al. Prosthetic Joint Infection. [Updated 2023 Apr 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448131/
- Infección de prótesis de rodilla o cadera: Diferencias entre aguda y crónica Blog del Dr. Guillem Bori Blog. (n.d.). Retrieved March 2, 2021, from https://www.barnaclinic.com/blog/protesis/infeccion-de-protesis-diferencias/.
- Infección de prótesis articular – Guía PRIOAM. (n.d.). Retrieved March 2, 2021, from https://guiaprioam.com/indice/infeccion-de-protesis-articular/.
- Infección de prótesis articulares. Diagnóstico y tratamiento. Clínica Universidad de Navarra. (n.d.). Retrieved March 2, 2021, from https://www.cun.es/enfermedades-tratamientos/enfermedades/infecciones-protesis-articular.
-
Tande, A. J., & Patel, R. (2014). Prosthetic joint infection. Clinical microbiology reviews, 27(2), 302–345. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3993098/
- Tenaglia, D. K. (n.d.). Infección de prótesis articulares. Retrieved from http://www.infectologia.edu.uy.
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.









