Description and Causes of Miosis (Pinpoint Pupils)


Written and verified by the doctor Leonardo Biolatto
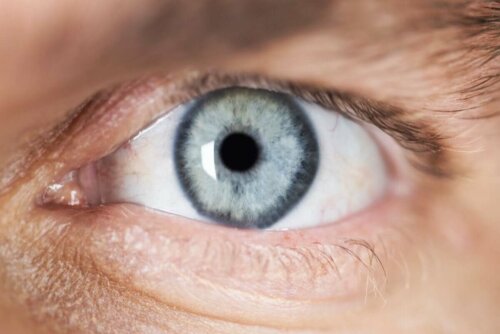
Miosis is the medical term used to refer to pinpoint pupils. In other words, it’s about the contraction of the pupil — it may seem irrelevant but actually reveals a lot about a person’s health.
This part of the eye reacts physiologically to changes in light by either contracting or dilating. In addition, its size changes when a person consumes toxins or when there’s brain damage. Thus, continue reading to find out everything you didn’t know you wanted to know about miosis.
Miosis (pinpoint pupils)
As we’ve just pointed out, miosis consists of the contraction of the pupil — the darkest part of the eye located in the center of the iris. It’s responsible for controlling the amount of light that passes into the eyeball, in the direction of the retina.
It dilates or contracts in order to adjust light, depending on how much of it there is in a given environment. Thus, it dilates when the environment is dark — this is called mydriasis. In contrast, the pupils get smaller when there’s a lot of light. This is a normal, physiological reflex controlled by the parasympathetic nervous system.
These movements are due to the ciliary muscle, the iris dilator present in the eye. The sympathetic nervous system coordinates the action.
Causes of pinpoint pupils
As we explained above, miosis is a physiological process that occurs in response to the amount of light. However, it isn’t the only situation that can lead to this reaction. Certain substances or diseases can cause it as well and that we’re about to describe.
Opioid consumption
Opiates alter the central nervous system. People either use them as medication for a given condition or for recreational purposes. Fentanyl, morphine, heroin, and methadone are just some of them.
They depress the nervous system and so the pupils contract and hardly react to light stimuli. According to an article published in Universidad Libre Seccional Barranquilla, opioid intoxication is characterized by miosis, and respiratory and consciousness depression, among other signs.
Intoxication by chemicals
In addition to opioids, there are many other chemicals that can lead to miosis. In fact, several medications list it among their side effects — antipsychotics such as haloperidol, for example. The same is true for topical drugs used for treating glaucoma.
Horner’s syndrome and miosis
The symptoms of this condition appear after a nerve injury. It causes myosis and a droopy eyelid. In addition, it decreases sweating on that side of the affected face.
According to an article published in Acta Médica del Centro, iatrogenesis is one of the main causes of this syndrome. That is, it happens as a result of medical failure after facial surgeries and dental or therapeutic interventions applied for trigeminal neuralgia.
Check out these Keys to Protecting Your Eyes During the Summer
Cerebral hemorrhage
In some cases, miosis may appear depending on the area of the brain affected by bleeding. In cases of a serious stroke or when the thalamus is involved, for example.
Pancoast tumor
This type of cancer occurs in the lung and can affect parts of the sympathetic nervous system — responsible for producing mydriasis, the opposite of myosis. Thus, the pupil cannot dilate and remains contracted as a result.
Read about the Four Exercises For Eye Health
Diagnosis of pinpoint pupils
In order to diagnose the cause of miosis, the simplest thing to do is look at the general condition of a given patient. Many of the etiologies that produce the symptom, such as opioid poisoning or cerebral hemorrhage, are usually accompanied by an alteration in the level of consciousness.
Ideally, ask the person if they’re under the effect of drugs or medications if they’re conscious. Also, look at how the pupils react to light stimuli. A doctor or nurse will test various eye reflexes to check the neurological state.
The photo motor reflex is among them, which consists in observe if the pupil contracts more when exposed to the light. Another one is the consensual reflex, which confirms if the pupil of the other eye (the one not being illuminated) is also contracting. This shows whether the injury is in one of the peripheral nerves or in the upper brain.

A physiological reflex
Miosis or pinpoint pupils is a physiological mechanism that occurs in response to light. However, it can also be secondary to neurological damage or intoxication by certain substances.
Thus, it’s an essential part of the medical examination and provides a lot of information about a patient’s condition. You must suspect an underlying pathological process when the sign is persistent.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- Síndrome de Claude-Bernard-Horner. Presentación de un caso. (n.d.). Retrieved September 7, 2020, from https://www.medigraphic.com/cgi-bin/new/resumen.cgi?IDARTICULO=39027
- Exploración de los reflejos pupilares | Oftalmología en la práctica de la medicina general, 4e | AccessMedicina | McGraw-Hill Medical. (n.d.). Retrieved September 7, 2020, from https://accessmedicina.mhmedical.com/content.aspx?bookid=1498§ionid=99962670
- Filippa, R., Toso, A., Cordero, J., & Olivos, P. (n.d.). Intoxicacion por Haloperidol (Haldol ).
- Vista de Intoxiación opioide | Biociencias. (n.d.). Retrieved September 7, 2020, from https://revistas.unilibre.edu.co/index.php/biociencias/article/view/2783/2203
- Panagopoulos, Nikolaos, et al. “Pancoast tumors: characteristics and preoperative assessment.” Journal of thoracic disease 6.Suppl 1 (2014): S108.
- Carrera, Maria Alicia Vera, et al. “Manejo de intoxicación por opioides.” RECIMUNDO 3.4 (2019): 494-510.
- Garófalo, Mariano, and Germán Píccolo. “CAPÍTULO 3 Efectos oculares adversos provocados por medicamentos.” Manual práctico: optometría clínica: 43.
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








