What Causes Inflamed Lymph Nodes?

Written and verified by psychologist Valeria Sabater
First of all, it is important to know that many cases of inflamed lymph nodes are not serious, especially if they are due to infections. However, it is always advisable to control the state of your lymph nodes in order to prevent other diseases. If they do become inflamed, it is best to see a doctor.
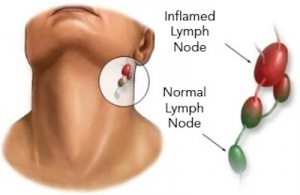
These small lumps that sometimes appear as small swellings on your neck, like when you have a cold for example, are called lymph nodes. They are essential for your body and act as liquid filters for the lymph tissue. They are shaped like almonds, barely more than a half an inch, and form around your neck, armpits, groin, thorax, and abdomen.
If you notice that they are inflamed, the first thing you should do is keep calm and remember that over half of the time it is due to normal processes. However, it is always best to get a diagnosis from a doctor. We’ll now explain the function of the lymph nodes and the causes of inflammation.
What do lymph nodes do?
This is basically what lymph nodes do:
- In the first place, they filter the lymph nodes from foreign substances like bacteria and cancerous cells, and destroy them.
- Additionally they produce white blood cells, like lymphocytes and plasma, which are responsible for destroying foreign substances
- They have an important part to play in defending your immune system.
Lymph nodes have different shapes and sizes. For example, underneath the jaw they are flat and around 0.4 inches wide and in the shape of a bean. The ones in the nape are around 0.2 inches, and are shaped like a lentil. And the lymph nodes in the groin are long, and a little over 0.6 inches wide.
Why do I get inflamed lymph nodes?
There are many reasons for inflamed lymph nodes. Since their main function is to protect your immune system, they are very sensitive to any changes. It could be due to insignificant causes or have more serious origins, like cancer, for example. But let’s look at the possible causes of inflammation in detail:
- Normal infections due to colds, flus, or tonsillitis
- Specific bacterial infections: syphilis, tuberculosis, salmonella food poisoning
- Lupus infections
- Viral infections like rubeola, measles
- Infections from other bacteria which causes malaria and leishmaniasis
- Rheumatic diseases
- Inflammation of lymph nodes due to medications: perchlorate, cotrimoxazole, hydantoin
- Stress, sleeping poorly, bad diet, lack of nutrients
- Sometimes lymph nodes can get inflamed due to lymphoma. These are tumorous diseases that doctors treat in the same way as benign neoplasms (non-cancerous). However, you have to keep in mind that there is a risk of malignant lymphoma, and your doctor will carefully monitor any changes or symptoms.
Initial evaluations of your lymph nodes
Your doctor will obviously carry out a diagnosis and tell you the steps to take. Nevertheless, you should always ask yourself the following questions:
- Have you had a cold or flu?
- Where is the inflamed lymph node? In the neck, armpit, collarbone?
- When did you begin to notice it? Was it sudden or did it grow little by little?
- Is it painful?
- Have you had previous illnesses?
- Do you take any medications?
- Have you recently gone on vacation?
- Have you lost weight?
All of this will allow you to detect which part of your immune system hasn’t recovered yet, as most of the time inflammation in lymph nodes comes from previous illnesses. Sometimes it is also because of medication or bacteria. With this information and the proper tests, your doctor will be able to tell you the cause of the swelling.
Things to keep in mind
In most cases of inflamed lymph nodes, the problem occurs in the neck and the origin is almost always due to neck or mouth infections. These are not very serious. However, you should make sure that the lump doesn’t grow excessively. If it approaches 2 inches in diameter, you will have to do a biopsy.
Remember that although the nodes in your neck are normally harmless, the ones located in the collarbone area, no matter their size, are always considered to be dangerous. You will need to treat these urgently, because they tend to lead to cancerous growths.
How to care for and prevent lymph node problems

One of the keys for preventing inflamed lymph nodes as much as possible is undoubtedly strengthening your immune system. That is why it is important to eat the following foods daily:
Vitamin C
This is essential for your immune system. It fights infection and viruses, and protects your cells. You can find it in citrus fruits, kiwis, strawberries, mangos, tomatoes, etc.
Vitamin E
It increases white cell production, which helps to protect you from cancer and bacteria. It is found in most fruits, vegetables, and nuts, like walnuts, pistachios, almonds, etc.
Foods Rich in Betacarotene
These have antioxidants, fight free radicals, and strengthen your defenses. It is essential to eat foods like carrots, corn, watermelon, cabbage, beets, pumpkin, asparagus, apricots, etc.
Selenium and Zinc
These help you produce more cells, which, in turn, strengthen your immune system. What foods contain selenium and zinc? Whole grains, Brazil nuts, most other nuts, seafood, soybeans, among others.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- García-Aguado, J. (2010). Estudio del paciente con adenopatías periféricas. Séptimo Curso de Actualización Pediatría. Madrid, España: Exlibris Ediciones, 31-42. https://www.academia.edu/36166258/Estudio_del_paciente_con_adenopatias_perifericas
- Maini, R. & Nagalli, S. (2021). Lymphadenopathy. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK558918/
- Mauro-Martín, S. y Garicano-Vilar, E. (2015). Papel de la vitamina C y los β-glucanos sobre el sistema inmunitario: revisión. Revista Española de Nutrición Humana y Dietética, 19(4), 238-245. Disponible en: https://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S2174-51452015000400008
- Rizvi, S., Raza, S. T., Ahmed, F., Ahmad, A., Abbas, S., & Mahdi, F. (2014). The role of vitamin E in human health and some diseases. Sultan Qaboos University Medical Journal, 14(2), 1-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3997530/
- Casares Diaz, S. A., Milanesio, M., Amelia, E. M., Saad, E. J., Guanchiale, L., & Alomar, J. M. (2021). Linfohistiocitosis hemofagocítica como presentación de Linfoma de células-T. [Hemophagocytic lymphohistiocytosis as a presentation of T-cell lymphoma]. Revista de la Facultad de Ciencias Medicas (Cordoba, Argentina), 78(3), 317–321. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8760911/#:~:text=La%20linfohistiocitosis%20hemofagoc%C3%ADtica%20es%20un%20s%C3%ADndrome%20hiperinflamatorio%20que%20puede%20ser,el%20manejo%20de%20estos%20pacientes.
- Castañeda, N., Narro, F., & Fortes G. (2020). Linfadenopatía cervical en pediatría. Revista Latinoamericana de Infectología Pediátrica, 33(1), 44-48. https://www.medigraphic.com/cgi-bin/new/resumen.cgi?IDARTICULO=92385
- Null M, Arbor TC, Agarwal M. (2023). Anatomy, Lymphatic System. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK513247/
- Chaves, W. G., Carrero, N. E., & Tejeda, M. (2015). Linfadenopatías generalizadas como primera manifestación de lupus eritematoso sistémico; un diagnóstico diferencial de enfermedad linfoproliferativa. Un reporte de dos casos. Revista Colombiana de Reumatología, 22(4), 225-230. https://www.elsevier.es/es-revista-revista-colombiana-reumatologia-374-articulo-linfadenopatias-generalizadas-como-primera-manifestacion-S0121812315000833
- Diccionario de cáncer del NCI. (s. f.). Instituto Nacional del Cáncer. Consultado el 31 de mayo de 2023. https://www.cancer.gov/espanol/publicaciones/diccionarios/diccionario-cancer/def/ganglio-linfatico
- Palmezano-Díaz, J. M., Figueroa-Pineda, C. L., Rodríguez-Amaya, R., & Plazas-Rey, L. K. (2018). Prevalencia y caracterización de las enfermedades autoinmunitarias en pacientes mayores de 13 años en un hospital de Colombia. Medicina interna de México. https://www.scielo.org.mx/scielo.php?script=sci_arttext&pid=S0186-48662018000400003
- Zambrano-Ferreira, J. A., Pérez-Fonseca, S. V., Caro-Becerra, A. C., González-Rocha, Y. F., Gelvez-Díaz, J. M., Rueda-Gutiérrez, J. A., & Mallarino, G. (2021). Linfedema: de la fisiopatología al tratamiento actual. Médicas UIS, 34(3). http://www.scielo.org.co/scielo.php?script=sci_arttext&pid=S0121-03192021000300061
- Villegas-Molina, J. P., Yarce-Prince, M., Ochoa-Hernández, J. L., De Dios Cardona-Muñoz, S., Orozco-Beltrán, L. V., De Jesús Ruiz-Hernández, E., Cárdenas-Cañas, C. A., Correa-Londoño, L. A., Atencia-Flórez, C. J., & Velásquez-Lopera, M. M. (2019). Enfoque del paciente con adenopatías generalizadas. Importancia de la estrategia didáctica del estudio de casos clínicos: a propósito de un paciente con linfoma de Hodgkin asociado a una infección por el virus de Epstein-Barr. Iatreia, 32(4), 328-337. http://www.scielo.org.co/scielo.php?script=sci_arttext&pid=S0121-07932019000400328
- Qiu, F., Liang, C. L., Liu, H., Zeng, Y. Q., Hou, S., Huang, S., Lai, X., & Dai, Z. (2017). Impacts of cigarette smoking on immune responsiveness: Up and down or upside down?. Oncotarget, 8(1), 268–284. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5352117/
- Le, C. P., & Sloan, E. K. (2016). Stress-driven lymphatic dissemination: An unanticipated consequence of communication between the sympathetic nervous system and lymphatic vasculature. Molecular & cellular oncology, 3(4), e1177674. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4972108/
- Herrera, M., Molina, P., & Souza-Smith, F. M. (2021). Ethanol-induced lymphatic endothelial cell permeability via MAP-kinase regulation. American journal of physiology. Cell physiology, 321(1), C104–C116. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8321794/
- Villagran Orellana, M., Martínez Sanguinetti, M. A., Díaz, F., Petermann-Rocha, F., & Celis-Morales, C. (2020). Nutrientes, alimentación y actividad física como potenciadores del sistema inmune en tiempos de COVID-19.: Nutrients, diet, and physical activity as enhancers of the immune system in times of COVID-19. ARS MEDICA Revista De Ciencias Médicas, 45(4), 48–60. https://www.arsmedica.cl/index.php/MED/article/view/1732
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.









