Antiphospholipid Syndrome: Causes, Symptoms, and Treatments

Written and verified by the doctor Mariel Mendoza
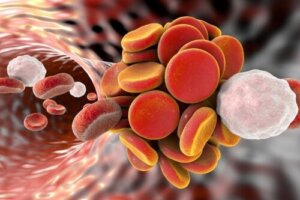
Antiphospholipid syndrome occurs when the immune system creates antibodies that attack the body’s own tissues (autoantibodies). As a result, blood clots form in the arteries and veins , preventing proper blood flow. This results in symptoms associated with decreased or obstructed flow.
In particular, it often manifests with episodes of thrombosis and repeated miscarriages. Unfortunately, there’s no specific cure for this syndrome. However, several medications are available that reduce clot formation and other associated complications. Want to know more about it? Read on!
The cause of antiphospholipid syndrome is not well defined
Antiphospholipid syndrome can occur due to an underlying disease, such as an autoimmune disorder. However, there are cases in which this cause doesn’t exist. It may have an associated genetic component, as is the case with most autoimmune diseases.
Systemic lupus erythematosus is the condition most associated with its occurrence. However, other conditions also increase the risk of blood clots produced by autoantibodies. These include the following:
- Pregnancy
- Prostration
- Surgeries
- Tobacco smoking
- Taking oral contraceptives or estrogen replacement therapy at menopause
- High triglyceride and cholesterol levels
How is the diagnosis made?
The diagnosis is made by serological measurement of autoantibodies. These must appear at least twice consecutively in the blood in tests performed 12 or more weeks apart. Nowadays, different types of autoantibodies are measured:
- Anti-cardiolipin
- Anti-β2-glucoprotein I
- Lupus anticoagulant
- Other antiphospholipid antibodies that aren’t usually measured routinely
However, it’s possible to have the presence of antiphospholipid autoantibodies and have no symptoms. The diagnosis is confirmed only in the presence of autoantibodies and clinical manifestations (thrombosis or pregnancy complications).
The symptoms of antiphospholipid syndrome
The clinical manifestations of this syndrome depend on where the blood clots are lodged. Complications include the following:
- Renal insufficiency
- Cerebrovascular disease
- Pulmonary or cardiovascular problems
- Pregnancy difficulties
How autoantibodies generate thromboembolism
The autoantibodies present in antiphospholipid syndrome act – as the name suggests – against one’s own tissues. Thus, they increase the risk of blood clot formation due to cell damage in the blood vessels.
However, thrombosis doesn’t usually occur in the absence of other conditions that promote clottings, such as prolonged inactivity, prostration, pregnancy, or recent surgery. Other risk factors include the following:
- Estrogen use
- Associated autoimmune diseases
- Obesity
- Alteration of lipid profiles
- Arterial hypertension
- Hardening of the arteries (atherosclerosis)
Antiphospholipid syndrome can affect any vascular bed
Thrombosis in antiphospholipid syndrome can occur anywhere in the cardiovascular system. Thus, it can affect any organ of the body. Symptoms will depend on where it occurs.
In addition, there are other associated conditions, such as a decrease in the number of platelets (thrombocytopenia). This is due to the number of blood cells that are used in the production of clots. This increases the likelihood of bleeding, especially in the nose and gums.
It’s also possible to experience marbled skin (“blotchy” skin or livedo reticularis ) and skin ulcers.
Clinical manifestations according to affected organs
- Kidney failure due to thrombosis of large vessels or glomerular capillaries (thromboembolic microangiopathy).
- Deep vein thrombosis. This manifests with pain, swelling, and redness in the lower limbs.
- Pulmonary embolism due to the migration of a clot into the respiratory circulation. When a clot lodges in the lung, it is manifested by a sudden shortness of breath, chest pain, and a cough with expectoration of blood.
- Cerebrovascular disease or transient ischemic attack, which depends on the extent of involvement of the central nervous system circulation. It may present as paralysis or weakness of the face, arm, or leg; visual disturbances or slurred speech; and a sudden, severe, generalized headache.
- Cardiovascular disease due to obstruction of the coronary circulation (may produce infarction). They can also lodge in the heart valves and travel through the bloodstream (arterial embolism) or damage and thicken them.
- Other neurological conditions due to decreased blood flow such as migraines, seizures, and chorea.
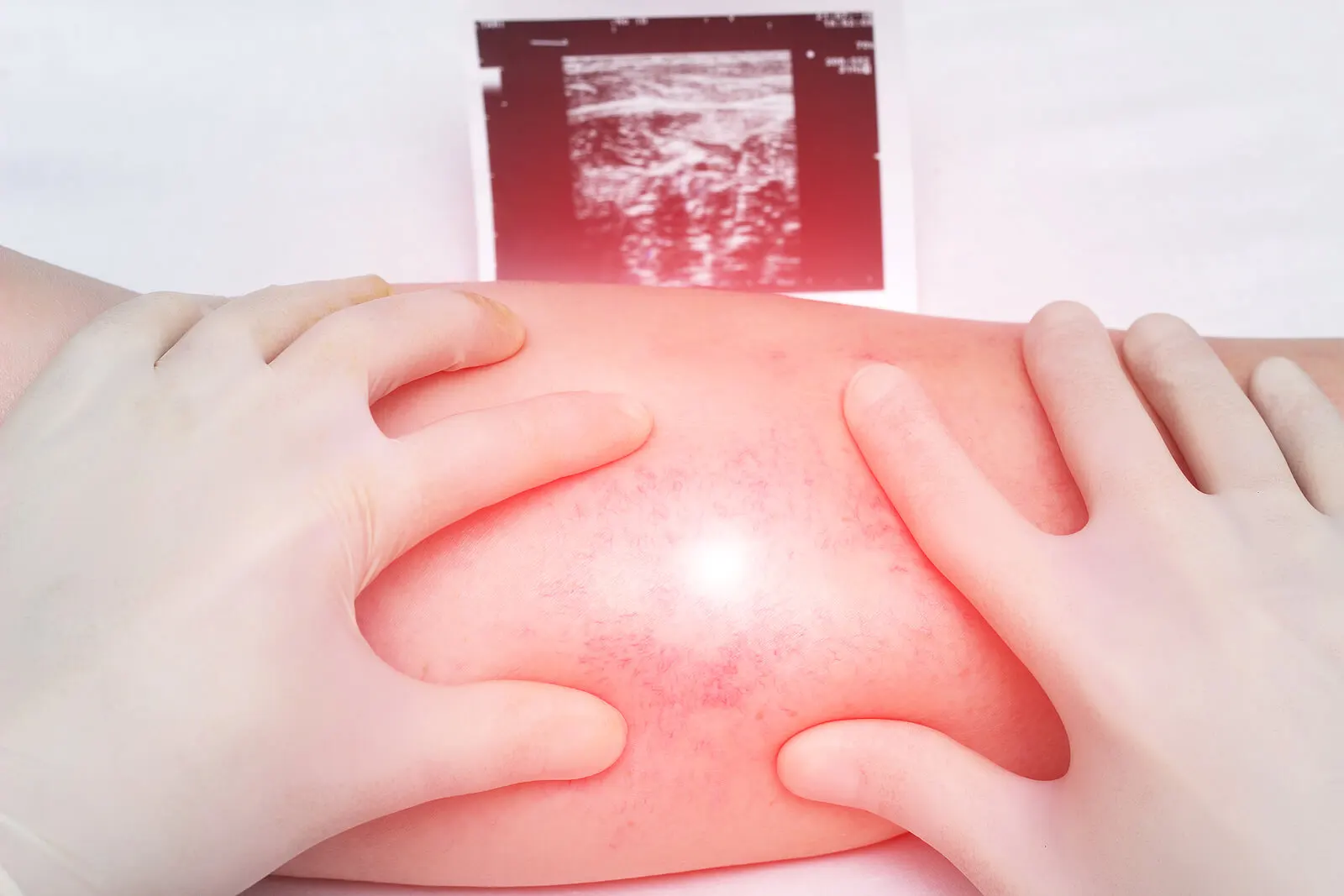
- In pregnancy , complications range from repeated miscarriages to intrauterine fetal death. In addition, it can lead to preeclampsia (increased blood pressure with loss of protein in the urine), intrauterine growth restriction, and preterm delivery.
We think you may be interested in reading this, too: 7 Natural Ways to Boost Your Immune System and Prevent Colds and the Flu
Treatment of antiphospholipid syndrome
Treatment of antiphospholipid syndrome is based on preventing clot formation through the use of oral anticoagulant (blood thinning) or antiplatelet drugs. In addition, risk factors associated with thrombosis should be addressed.
Cases of acute thrombotic episodes are initially managed with intravenous heparin, followed by oral anticoagulants (warfarin). The use of anticoagulants should be monitored with a blood test to decrease the risk of bleeding, either through a wound or under the skin.
After treating the acute event, people with this syndrome should take oral anticoagulants to prevent the reoccurrence of blood clots in the veins. To avoid arterial periods, antiplatelet drugs such as aspirin and clopidogrel are usually used.
In the case of pregnant women, it’s possible to carry the pregnancy to term with proper monitoring and the use of medications. Treatment includes heparin or heparin with low-dose aspirin because warfarin cannot be administered in these cases because it can affect the fetus.
Women of childbearing age with antiphospholipid syndrome who wish to conceive should also take low-dose aspirin.
Like this article? You may also like to read: The Role of Zinc in Strengthening Your Immune System
What to remember?
The presence of one or more episodes associated with the formation of blood clots or repeated pregnancy loss (or other pregnancy complication) that can’t be explained by another cause should raise a suspicion of antiphospholipid syndrome. Although it has no specific cure, the symptoms of this condition can be controlled. It’s even possible to carry a pregnancy to term. Therefore, in case of suspicion, it’s best to consult a rheumatologist as soon as possible.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- Bustamante JG, Goyal A, Singhal M. Antiphospholipid Syndrome. [Updated 2022 Jul 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430980/
- Aziz M, Iheanacho F, Hashmi MF. Physiology, Antibody. [Updated 2022 May 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK546670/
- Negro M. Síndrome antifosfolipídico. Suplemento 2012;16. Disponible en https://www.sah.org.ar/revistasah/numeros/vol16_supl2012_19_20.pdf
- Porcel J. Manejo del Síndrome Antifosfolipídico. Clínica-UNR.org 2006. Disponible en http://www.clinica-unr.com.ar/2015-web/Especiales/15/Especiales%20-%20Porcel%20-%20AAF.pdf
-
Bienaimé F, Legendre C, Terzi F, Canaud G. Antiphospholipid syndrome and kidney disease. Kidney Int. 2017 Jan;91(1):34-44. doi: 10.1016/j.kint.2016.06.026. Epub 2016 Aug 21. PMID: 27555120.
- Farmer-Boatwright MK, Roubey RA. Venous thrombosis in the antiphospholipid syndrome. Arterioscler Thromb Vasc Biol. 2009 Mar;29(3):321-5. doi: 10.1161/ATVBAHA.108.182204. PMID: 19228605.
- Na YS, Jang S, Hong S, Oh YM, Lee SD, Lee JS. Clinical Phenotype of a First Unprovoked Acute Pulmonary Embolism Associated with Antiphospholipid Antibody Syndrome. Tuberc Respir Dis (Seoul). 2019 Jan;82(1):53-61. doi: 10.4046/trd.2018.0045. PMID: 30574689; PMCID: PMC6304333.
-
Atanassova PA. Antiphospholipid syndrome and vascular ischemic (occlusive) diseases: an overview. Yonsei Med J. 2007 Dec 31;48(6):901-26. doi: 10.3349/ymj.2007.48.6.901. PMID: 18159581; PMCID: PMC2628175.
- Soltész P, Szekanecz Z, Kiss E, Shoenfeld Y. Cardiac manifestations in antiphospholipid syndrome. Autoimmun Rev. 2007 Jun;6(6):379-86. doi: 10.1016/j.autrev.2007.01.003. Epub 2007 Jan 31. PMID: 17537384.
-
Di Prima FA, Valenti O, Hyseni E, Giorgio E, Faraci M, Renda E, De Domenico R, Monte S. Antiphospholipid Syndrome during pregnancy: the state of the art. J Prenat Med. 2011 Apr;5(2):41-53. PMID: 22439075; PMCID: PMC3279165.
- Galli M. Treatment of the antiphospholipid syndrome. Auto Immun Highlights. 2013 Dec 22;5(1):1-7. doi: 10.1007/s13317-013-0056-5. PMID: 26000150; PMCID: PMC4389011.
-
Adediran S, Agostino N. Coexistence of Antiphospholipid Syndrome and Heparin-Induced Thrombocytopenia in a Patient with Recurrent Venous Thromboembolism. Case Rep Hematol. 2017;2017:3423548. doi: 10.1155/2017/3423548. Epub 2017 Apr 26. PMID: 28589046; PMCID: PMC5424171.
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








