90% of Spaniards Carry the Varicella-zoster Virus


Written and verified by the doctor Leonardo Biolatto
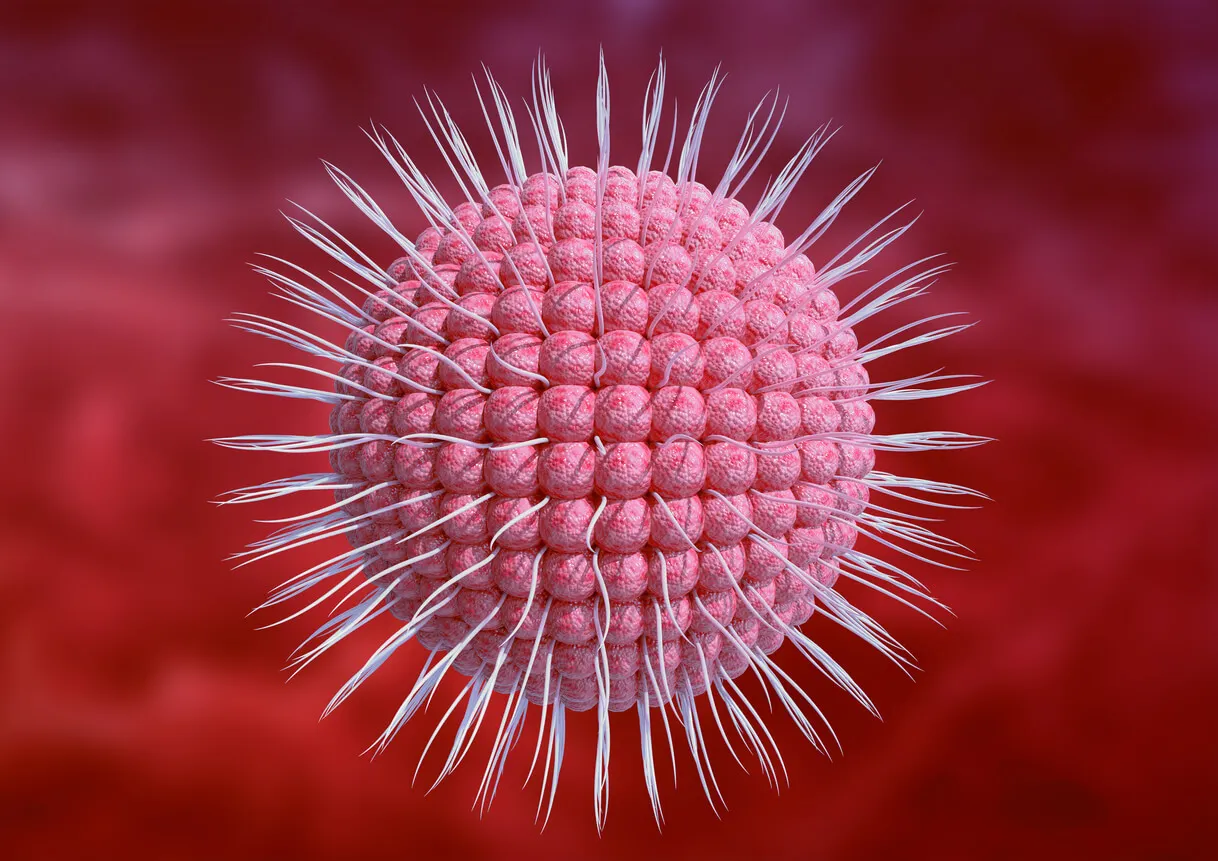
The varicella virus – more specifically named “varicella-zoster virus” – doesn’t just case the childhood rash disease known as chickenpox. It’s also responsible for shingles, or herpes zoster. Shingles is a disease that 30% of people over the age of 50 will develop at least once during their lifetime.
However, if we talk about the varicella-zoster virus, the statistics are even more telling. More than 90% of people over the age of 14, at some point in their lives, have come into contact with this viral agent.
Is shingles dangerous, and is there any way to eliminate the virus once it has become latent in the body? We’ll take a look at these questions in this article.
The surprising statistics of shingles
According to the scientific study by Cintia Muñoz-Quiles and collaborators, one in three people over the age of 50 develop the herpes zoster virus, colloquially known as shingles. At the same time, one in 10 of the same age group will have post-herpetic neuralgia (the intense pain that persists at the site of shingles after the lesions have disappeared).
The authors also point out that people with compromised immune systems are at greater risk. These immunocompromised patients may be up to 50% more likely to develop herpes zoster than the rest of the population.
Spain, in particular, reports up to 559 new cases of herpes zoster per 100,000 inhabitants in some communities. In fact, the figure becomes more prevalent the older people are in the studies.
From the age of 60 onwards, those who have had chickenpox in childhood are more likely to suffer from a reactivation of the virus, which has remained latent in the body. In fact, one in 5 people will go through this reactivation. And once they have had shingles, 6% of that group will get it again.
We think you may also enjoy reading this article: Somatization and Coronavirus: Believing You Have Symptoms Without Being Infected
What are shingles?
Shingles are the reactivation of the varicella-zoster virus that has become dormant in the body. Once a human being has been infected (something which almost always occurs in childhood), the viral agent remains in the body inactive, specifically in the neurons.
It can remain there for decades. It’s not even necessary for the person to have noticed the chickenpox infection in childhood. Even asymptomatic cases or those with mild signs are susceptible to the virus “hiding” and remaining latent.
In a situation of lowered defenses, due to stress, drugs, or age, the virus reactivates. It causes a rash with small blisters that can appear in different areas of the body, such as the intercostal space, the back, and even the face (eyes, ears, and mouth).
This is the well-known shingles disease. It includes the characteristic burning, burning, and intense pain along the path of the blisters. This coincides with the path of the affected nerve.
It’s common for the pain to appear before the outbreak. Once the vesicles appear, they begin to break down asynchronously, crusting over where they were. After 14-21 days, the scabs fall off spontaneously.
Sometimes there’s also a fever,but not always. There may also be some muscle aches or headaches.
Less common presentations of herpes zoster are those located on the face and abdomen. In particular, the ocular form is among the most painful manifestations of this virus.
Like this article? You may also like to read: How to Wash Fruits and Vegetables During the Coronavirus Pandemic
Post-herpetic neuralgia, a dreaded complication
The normal and expected course of shingles is around one month. After that time, most patients no longer have symptoms, and all skin lesions have disappeared.
However, up to one-third of those affected may develop a complication known as postherpetic neuralgia. This is a very intense pain that persists, despite the disappearance of the blisters.
The burning sensation may even last for more than three months in this complication, and patients also have increased sensitivity in the area. Even rubbing against clothing can intensify the discomfort.
It’s clear that the quality of life is greatly affected, especially because of its prolongation in time. In fact, it can reach up to four years in the most severe cases.

Is there any treatment for this virus?
The diagnosis is usually confirmed by the rash on the skin, although in some cases, confirmation is made by specific tests.
Antiviral treatments are available and should be used within 72 hours of the onset of shingles. It’s also recommended to keep the rash clean and dry to avoid a secondary skin infection.
Currently, there is no cure to eliminate the virus from our body, but it is a preventable disease.
What should I do if I suspect I have shingles?
Once the symptoms of shingles begin, the best thing to do is to consult a healthcare professional to begin treatment. Early antiviral agents may reduce the length of time your symptoms last.
At home, each patient should be responsible for caring for their wounds caused by the blisters and vesicles. The skin should be kept dry to avoid superinfections.
This is a condition that requires a lot of patience to go through. That’s why it’s important to be informed and follow the recommendations of professionals.
For more information, make sure to consult www.virusherpeszoster.es.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- Hadley, Graham R., et al. “Post-herpetic neuralgia: a review.” Current pain and headache reports 20.3 (2016): 1-5.
- Le, Phuc, and Michael Rothberg. “Herpes zoster infection.” Bmj 364 (2019).
- Mizukami, Akiko, et al. “Impact of herpes zoster and post-herpetic neuralgia on health-related quality of life in Japanese adults aged 60 years or older: results from a prospective, observational cohort study.” Clinical drug investigation 38.1 (2018): 29-37.
- Muñoz-Quiles, Cintia, et al. “Herpes zoster risk and burden of disease in immunocompromised populations: a population-based study using health system integrated databases, 2009–2014.” BMC infectious diseases 20.1 (2020): 1-14.
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








