7 Tips for Coping with Lupus Related Fatigue


Written and verified by the doctor Mariel Mendoza
People with lupus related fatigue have difficulty performing basic daily tasks, such as getting out of bed, eating and going to work. Eventually, other leisure activities (physical exercise or simply socializing) become complicated.
In people with systemic lupus erythematous, fatigue tends to be the initial symptom in up to half of the cases. It may be accompanied by irritability, tiredness, drowsiness, depression, and anxiety.
What is lupus-related fatigue?
Common fatigue and severe fatigue are very common in lupus. They could be due to the states of depression and anxiety characteristic of the disease.
Currently, the Fatigue Scale for Cognitive and Motor Function (FSMC) is used to address the symptom. It includes 20 variables that assess the functions separately. Then, the person is classified as mild, moderate, or severe, according to the results.
The fatigue factor is a value equal to or greater than 42 on the FSMC scale. And severe fatigue when it is equal to or greater than 63.
Fatigue can be seen as the overwhelming sensation of tiredness at rest. It prevents performing daily tasks, worsens with activity, and does not improve with rest.
Fatigue as a symptom is associated, in addition to the disease itself, with other factors:
- Depression and anxiety
- Being overweight or obese
- Sleep disorders
- Chronic anemia
- A sedentary lifestyle
- Fibromyalgia
All of these factors can aggravate fatigue in lupus or develop, some as a consequence. Extreme fatigue, for example, leads to a sedentary lifestyle, which increases the risk of obesity.

Daily tips for dealing with fatigue in lupus
If you are diagnosed with systemic lupus erythematous, you should know that tiredness and fatigue will appear. That’s why it’s good to implement some strategies to combat the symptom. Here are some tips that might help you.
1. Reduce your stress
Lupus fatigue improves as you work on relaxation techniques to manage stress. Yoga and meditation, balancing your workload, matching your activities to your physical abilities, and having regular rest and rest schedules are recommended.
2. Include daily exercise routines
Although people with lupus may have difficulty exercising, a sedentary lifestyle is a factor that aggravates fatigue. Regular exercise, on the other hand, allows muscles to become stronger, provides more energy, and improves mood.
Just by including 10 minutes of physical activity daily, the effects of stress and fatigue are reduced. In addition, it’s recommended to seek a balance between physical activity and rest periods.
Schedule other activities and down time outside your daily activities, including social gatherings, so you don’t run out of energy.
Aerobic physical exercise improves fatigue in lupus. Since this is a disease that involves multiple organs, such as muscles, skin, lungs, and joints, sports practice will influence cardiovascular risk.
Prolonged aerobic physical exercise programs have been shown to significantly decrease severe fatigue. Ideally, find a professional in the area who can show you some routines.
Check out these: 14 Exercises for People with Limited Mobility
3. Attend support groups and manage your emotions with therapy
Lupus fatigue could be due to depression and anxiety, as well as anger and frustration. Because letting these feelings evolve is counterproductive, you should try an approach through psychological therapy.
Being too tired to start or even complete any activity, as well as apathy, causes sadness that can be difficult to manage on your own. Also, participating in support groups lets us share with others going through the same problems.
4. Improve your sleep habits
Sleep disturbances can aggravate fatigue or be the cause because people with lupus often wake up feeling tired, even if they’ve slept for many hours. Interruption of sleep during the night and inability to return to sleep is also common.
7 to 8 hours of rest during the night is recommended. Naps should be short during the day so as not to affect nighttime sleep.
Exposure to screens at night should also be eliminated. Eat a light dinner 2 to 4 hours before bedtime. Do not consume caffeine and try relaxing music.
Create a relaxation routine before bedtime and try to wake up at the same time in the morning.
Sleep problems in lupus may be due to corticosteroid treatment in moderate to high doses. So, check with your doctor if you take these drugs.
5. Eat a balanced diet
A diet with adequate portions of protein and carbohydrates can combat lupus-related fatigue. Of course, people with this problem must give up toxic substances such as alcohol or tobacco.
Fatigue from lupus can also be due to a vitamin D deficiency, caused by a tendency to avoid sun exposure. Clinical studies have shown that within 6 months of implementing vitamin D supplementation, severe fatigue improves significantly in women with the disease.
Consult your physician if you require vitamin supplements.
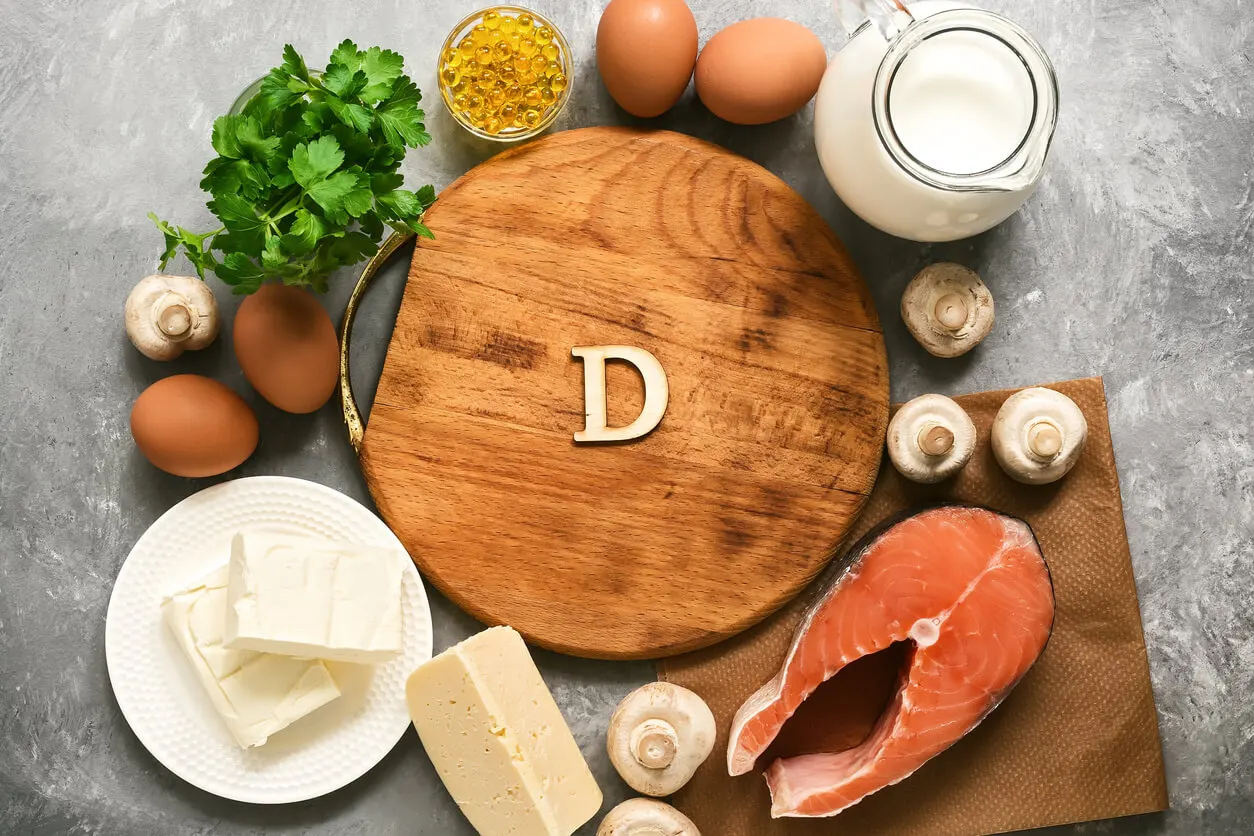
Read about: Vitamin D and Weight Loss: How Are They Related?
6. See your doctor to review your medication
Corticosteroids used as treatment can lead to insomnia, anxiety, and lupus-related fatigue. They can also affect the ability to achieve restful sleep.
Other treatments for lupus, such as anti-inflammatory pain relievers, antidepressants, and muscle relaxants, are capable of aggravating fatigue. This is why a regular evaluation of the therapeutic plan is necessary. Also, only a health professional can prescribe them.
7. Rule out other coexisting diseases
Lupus-related fatigue can worsen by the presence of other autoimmune, endocrine, or neurological disorders such as the following:
- Fibromyalgia
- Thyroid problems
- Renal insufficiency
- Anemia
If you present symptoms different from the usual or new ones, you should consult. Sometimes, the correction of an added pathology reduces the sensation of tiredness. For this, it’s essential to comply with the above advice of regular visits to the doctor.
Lupus-related fatigue requires professional evaluation
The first thing to do when faced with fatigue in lupus is to rule out the presence of an active phase of the disease. Thus, you must adjust treatment to seek remission of the acute period. It’s possible to increase the dose of the drugs already used or to add a different drug.
When there’s no high activity or acute episode of lupus, a doctor should evaluate other conditions that may promote fatigue. They should rule out concomitant anemia, renal failure, or thyroid problems.
Lupus-related fatigue can be debilitating, both physically and emotionally. It affects the ability to perform daily activities and requires medical help.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- Arnaud, L., Gavand, P. E., Voll, R., Schwarting, A., Maurier, F., Blaison, G., … & Martin, T. (2019). Predictors of fatigue and severe fatigue in a large international cohort of patients with systemic lupus erythematosus and a systematic review of the literature. Rheumatology, 58(6), 987-996. Disponible en https://academic.oup.com/rheumatology/article/58/6/987/5265278.
- Barbera I, et al. Prevalencia y factores asociados a fatiga en pacientes del sexo femenino con lupus eritematoso sistémico. Med Clinic (Barc) 2018;151(9):353-358. Disponible en https://www.sciencedirect.com/science/article/abs/pii/S2387020618304054
- Elera C, et al. Lupus eritematoso sistémico y fatiga. Rev. Cuerpo Med. HNAAA 2022;15(3). Disponible en https://www.cmhnaaa.org.pe/ojs/index.php/rcmhnaaa/article/view/1665/678.
- Mertz P, et al. Towards a practical management of fatigue in systemic lupus erythematosus. Lupus Science & Medicine 2020;7. Disponible en: https://www.researchgate.net/publication/347068650_Towards_a_practical_management_of_fatigue_in_systemic_lupus_erythematosus.
- Middleton, K. R., Moonaz, S. H., Hasni, S. A., López, M. M., Tataw-Ayuketah, G., Farmer, N., & Wallen, G. R. (2018). Yoga for systemic lupus erythematosus (SLE): Clinician experiences and qualitative perspectives from students and yoga instructors living with SLE. Complementary therapies in medicine, 41, 111-117.
- Sharif K, et al. Physical activity and autoinmune diseases: get moving and manage the disease. Autoinmune Reviews 2018;17(1):53-72. Disponible en https://www.sciencedirect.com/science/article/abs/pii/S1568997217302835.
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








