Skin Problems Caused by Stress

The skin is the body’s largest organ. As such, it can easily make many health problems visible, such as stress, which can lead to skin problems related to stress.
The skin: A mirror of your health
Unlike other organs and systems of the human body, you can check your skin at a glance. You can examine it without needing an x-ray machine, and easily detect any changes in your skin’s appearance.
Did you know that there’s a strong connection between the skin and the nervous system?
This connection starts at the embryonic stage and remains present even throughout adult life. When stress hormones are elevated, these cause a series of physiological changes in the body. These hormones also affect the skin.
Stress mechanisms are activated in the hypothalamus-pituitary axis, which releases different substances into the body. These substances have the job of activating the production of cortisol in the adrenal glands. If your stress hormones are high, this becomes visible on your skin.
The role of stress in skin problems

The body’s reaction to stress is a defense mechanism that the body uses to ensure its survival. A little stress is OK. However, when stress becomes chronic (constant high levels), it causes certain reactions throughout the whole body, including skin problems.
Overall, here are the most common effects stress has on the skin:
- Loss of elasticity
- Wrinkles
- Flabbiness
- Dull, tired-looking skin
- Discoloration
- Certain diseases
Skin problems caused by chronic stress generally have to do with blood circulation in the body. In a stressful situation, the body produces a quick response to the situation. It must react fast, and it does so with three options: fight, flight or paralysis, depending on the situation.
To provide the body with what it needs for these reactions, cortisol redirects the blood flow away from certain areas of the body and towards the muscles, heart, lungs, and brain. One of the areas of the body that suffers from this is the skin. Too much stress negatively affects the body’s immune system and makes the skin more vulnerable to infections and tumors. This is because the protection of the immune system processes slows down during the body’s reaction to stress.
Read also: Weakened Immune System: What to Look For
Cortisol and stress-related skin problems
During a stressful situation, the skin appears pale and dull. The lack of sufficient blood flow to the skin during stress is what causes skin problems. Cortisol also releases energy in the form of sugars that produce metabolic waste, which is known as free radicals. Free radicals are responsible for the appearance of wrinkles, frown lines, and pimples. They also make the skin fragile and dull looking.
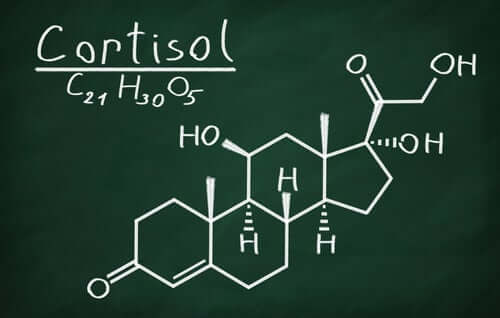
One of the skin problems that stress causes is premature aging. This is due to the further effects of cortisol in the body. Cortisol decreases the production of collagen, which affects the skin’s elasticity and causes wrinkles to appear. Also, it decreases the synthesis of melatonin, which is the hormone that regulates sleep. A deficiency in this hormone prevents the nightly regeneration of skin cells.
However, what about emotional influences? Do they also appear on the skin?
One example is in worry lines on the face. They say that the face is the mirror to the soul. Well, the emotional effects of stress often appear as wrinkles on the forehead and frown lines, which show the state of worry or discomfort.
Skin problems: Diseases that can appear with stress
Did you know that certain skin problems are directly linked to stress?
We’ve listed the most common among them here:
Acne
Although hormonal factors are normally held responsible for the appearance of acne, more and more importance is being attributed to emotional factors. When people improve their stress levels through medication, therapies, yoga, meditation and other remedies, their acne also significantly improves.
Discover more: 8 Steps for Eliminating Acne
Atopic dermatitis (or eczema)
Atopic dermatitis frequently appears due to such things as environmental factors, dehydration, irritants, infections, and even sweat. However, an astonishing 70% of cases are linked to stress.
A vicious cycle can develop between pruritus (itching) and scratching. These can become obsessive and cause dermatitis to worsen due to infection. Obsessive scratching can also make other more serious complications appear.

Eczema on neck
Seborrhoeic dermatitis
Episodes of stress are directly related to this skin disease. It can appear in people during times of extreme anxiety. Some examples may be when someone is changing jobs, moving house, planning a wedding or going through a divorce, during an illness or after the death of a family member, during exams, etc.
Excoriation disorder (skin picking)
With this disorder, the person compulsively scratches or picks at his or her skin, generating itching and scratching cycles that can last for years. It usually appears in younger people and is somewhat frequent in adolescent girls. Changes due to hormonal stress can provoke the disorder. The person may seriously injure themselves due to repeated scratching.
This skin disorder usually improves when emotional mood swings are treated. However, it can last for many years without treatment.
Alopecia areata (spot baldness)
This is the loss of hair on certain areas of the scalp. The bald patches are usually small circles about the size of coins. It is an auto-immune disease that can be genetic, but emotional factors are also a common influence.
The direct relationship of stress to auto-immune diseases is clearly demonstrated. It’s worth noting that according to certain studies, patients with alopecia areata are subject to stress in 30% to 90% of cases.

Psoriasis
Psoriasis is characterized by the acceleration of the normal life cycle of cells, which then die off early. They accumulate on the surface of the skin, forming scales and red spots. These produce intense itching and are very painful.
Psoriasis is a disease that has chronic episodes. That means that it may disappear for a while, but then when the patient is in stressful circumstances it can reappear. Stress levels, anxiety, and depression are all directly related to the severity of psoriasis episodes. Researchers have directly linked the degree of pruritus (itchiness) to the severity of depression that the patient suffers.

Improving a person’s stress levels usually lessens their tendency to anxiety and depression, and as a result outbreaks of psoriasis become less severe or common.
Finally, it’s worth mentioning that psoriasis can often cause a person to feel socially rejected or unacceptable. The patient feels stigmatized because of their appearance and can tend to try to hide the outbreaks, which in turn is another cause of stress that can make psoriasis worse.
Conclusion
We’ve seen just a few examples in this article of how stress can cause various skin problems. However, it’s always recommendable to try to manage stress and anxiety levels, even if you don’t suffer from skin problems.
In addition to causing anxiety and depression, chronic stress also eventually weakens the immune system, which can lead to many different disorders and diseases.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- Tribó M. Razones de ser y utilidad de la psicodermatologia. Piel 2006; 21:51-3
- Gracia M, Ruiz S. Estrés, calidad de vida y psoriasis: estado actual. Psiquiatr Biol. 2001;08:141-5.
- Castellano Rioja, E. Unidad didáctica V Bloque psicología 2ª parte. Master Deterioro Integridad Cutánea Ulceras y Heridas.
- García Hernández, M.J. y Ruiz Redondo, S. Suicidio y Dermatología. Actas Dermosifiliogr. 1999; 90:411-5
- Grimalt, T.; Cotterill, J.A y cols. Dermatología y Psiquiatría. Historias clínicas comentadas. Madrid. Aula Médica Ediciones 2002: 20-38.
- Romaní J, Chesa D. Psicodermatología en atención primaria. Piel. 2005;20(6):282-9
- Ricardo Alonso O, Rodríguez Sánchez M, Hernández Fernández M, Alonso González M. Aspectos de interés sobre dermatitis atópica, su diagnóstico y tratamiento. Rev.Med.Electrón. 2019; 41( 2 ): 496-507.
- Chen Y, Lyga J. Brain-skin connection: stress, inflammation and skin aging. Inflamm Allergy Drug Targets. 2014;13(3):177-90.
- Gil Díaz M, Boixeda de Miguel J, Truchuelo Díez M, Morais-Cardoso P. Rosácea: revisión y nuevas alternativas terapéuticas. SEMERGEN – Medicina de Familia. 2011;37(2):83-86.
- Gouin JP, Kiecolt-Glaser JK. The impact of psychological stress on wound healing: methods and mechanisms. Immunol Allergy Clin North Am. 2011 Feb;31(1):81-93.
- Silvestre-Salvador J, Serrano-Manzano M, Serra-Baldrich E, Palacios-Martínez D, Gómez-de la Fuente E, Heras-Hitos J et al. Recomendaciones para el manejo de la urticaria en Atención Primaria. Medicina de Familia SEMERGEN. 2020;46(4):270-276.
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.









