Recent Advances in the Treatment of Thrombocytopenia


Written and verified by the doctor Maryel Alvarado Nieto
Platelets, or thrombocytes, are part of the components that circulate in the blood. These elements are formed in the bone marrow from a large cell: the megakaryocyte. From there, they’re released into the bloodstream, where they help stop bleeding. In this article, we’ll discuss the treatment of thrombocytopenia, a condition in which the concentration of platelets is decreased.
Why is the thrombocyte count important?
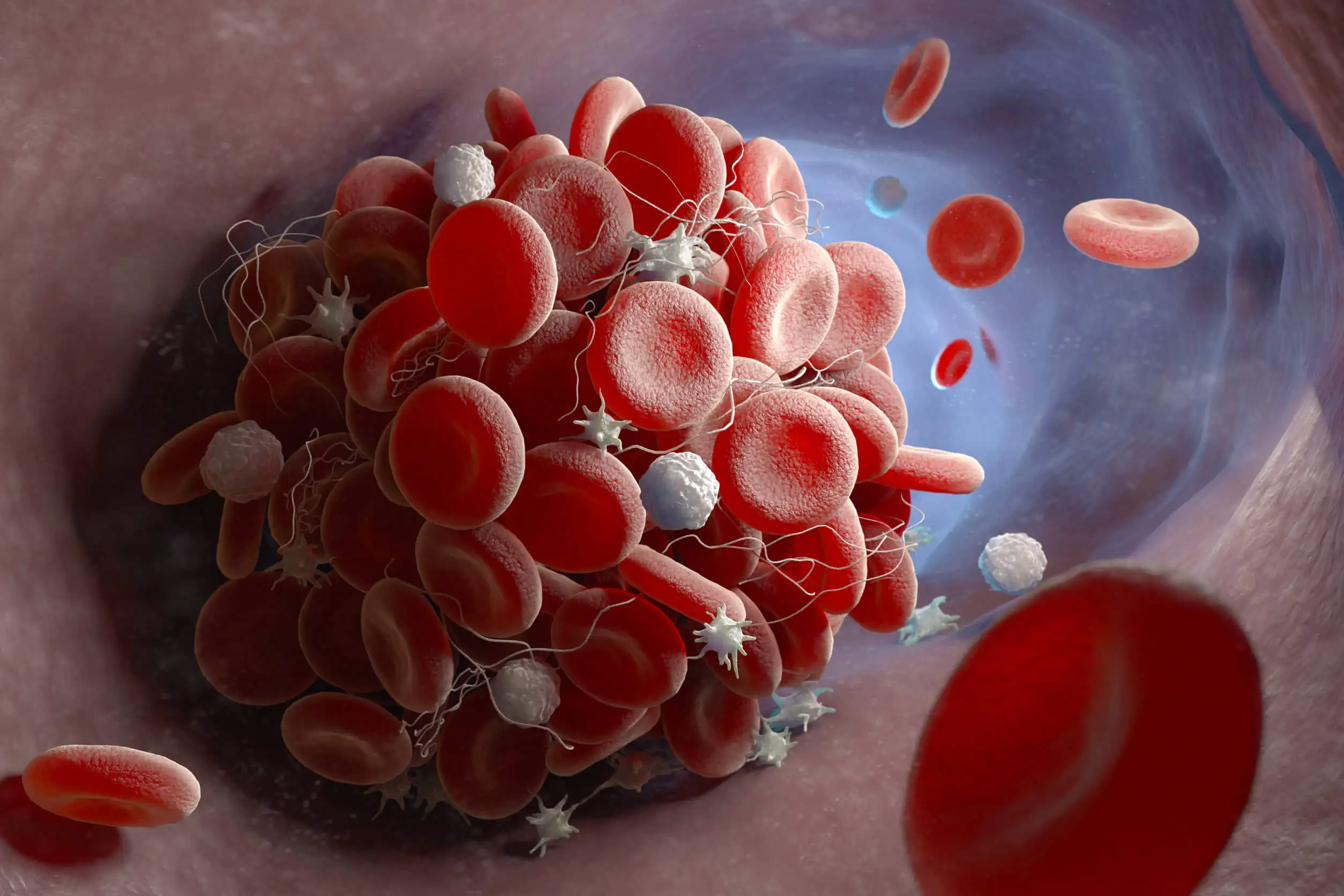
The main function of platelets is to participate in hemostasis, i.e. clotting. They do this by allowing thrombocytes to bind to each other, adhering to the injured blood vessel.
In this way, a clot is formed that prevents the blood from escaping. This is why the platelet concentration must remain within an established, normal range.
An excess of these elements in the circulation is a risk factor for a thrombotic event to occur. Conversely, a decrease in platelet count leads to an increased vulnerability to bleeding. This risk increases the lower the number of platelets in the blood.
What is thrombocytopenia?
Although the lower limit for platelet concentration is usually around 150 x109 thrombocytes/L, a figure of less than 100 x109 platelets/L is considered thrombocytopenia. In other words, less than 150,000 platelets per microliter of blood.
There are several conditions that cause a low thrombocyte count—however, the most common occurs because of a disorder of autoimmune origin.
It’s for this reason that the term thrombocytopenia is used almost synonymously with immune thrombocytopenia. This hematological disorder used to be known as idiopathic thrombocytopenic purpura (ITP), but nowadays this name is not recommended, since many patients don’t suffer from the characteristic cutaneous bleeding, purpura.
Even so, the acronym ITP is still used.
On the other hand, the mechanisms involved in producing this blood disorder are so diverse that there’s no consensus to explain the pathophysiology that causes it. The clinical manifestations of patients with thrombocytopenia confirm the great variability of factors involved.
Treatment of thrombocytopenia
In most cases, patients have little symptomatology and it’s usually mild to moderate. It is, therefore, advisable to treat thrombocytopenia on an individual basis. Furthermore, platelet concentration shouldn’t be the only factor taken into consideration.
On the other hand, there’s a general consensus on the goals of the different management options available. The main objective is to decrease the risk of bleeding by increasing the platelet count. However, different studies insist that no attempt should be made to bring this value to normal limits.
Such behavior wouldn’t only be unnecessary, but also detrimental to the patient, as the quality of life is also counted as an important factor in the treatment of thrombocytopenia. The adverse effects can never outweigh the potential benefits offered by the medication.
Therefore, therapeutics shouldn’t only mean an improvement in symptoms and a decrease in the risk of bleeding for the patient, but should also consider the safety profile of the substances used to manage the medical condition.
Conventional therapy: an obsolete treatment for thrombocytopenia?
Early attempts to control plateletopenia sought to inhibit the immune system. In this way, the mechanisms involved in the increased thrombocyte destruction seen in ITP were hindered. However, this approach puts the patient in a very vulnerable position, as it increases the risk of infection.
Conventional therapeutic guidelines include the following:
- Corticosteroids
- Human immunoglobulin
- Immunosuppressants
Chemotherapeutic and antibacterial agents are also used. Splenectomy (surgery to remove the spleen) is the last measure available.
Discover more: Blood Clots: Watch Out for These 8 Signs
What options are currently available?
Because immunosuppression isn’t an ideal treatment due to the high risk of infection, several researchers have looked for other molecules, with the aim of achieving safer therapeutics. These lines of research have been ongoing for more than a decade.
The COVID-19 pandemic has pushed the search for effective treatments with improved safety profiles compared to immunosuppressive therapies. The reason for this demand is clear: a suppressed immune system is a risk factor for triggering severe COVID infections.
This is why research is looking for specific molecules that can interact with some of the mechanisms involved in immune thrombocytopenia. For this, a broader understanding of these mechanisms is vital.
Thrombopoietin receptor agonists
There are two molecules that are being used to treat thrombocytopenia: romiplostim and eltrombopag. The purpose of these drugs is to stimulate the bone marrow to produce a greater number of platelets. So far, they have been shown to be effective and safe.
Despite these results, their use is only justified in cases where thrombocytopenia persists after treatment with conventional therapies. For this reason, these molecules are considered second-line agents.
To achieve greater acceptance by the medical community, more extensive research is needed to provide more information on the safety profile of the molecules.

Tyrosine kinase inhibitor (SYK)
Another treatment option for immune thrombocytopenia is fostamatinib, a molecule that prevents platelets from being destroyed by the immune system. This therapy is given orally and has shown good patient tolerance following its recent approval.
The response is positive, especially for some people with a history of ineffective conventional therapies. On the other hand, the adverse effects described are usually mild to moderate. These include high blood pressure and diarrhea.
Searching for a treatment for thrombocytopenia: looking to the future
Finally, new treatment prototypes are in various stages of clinical research. Some of them have shown encouraging results, but with the caveat that the studies include small groups of patients. It is for this reason that both older treatments and new therapeutic proposals should be carefully evaluated.
Similarly, all of this research has been made possible by a better understanding of the mechanisms involved in thrombocytopenia. Therefore, achieving more effective and safer therapies seems to be a near possibility.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- Bidika, E., Fayyaz, H., Salib, M., Memon, A. N., Gowda, A. S., Rallabhandi, B., & Cancarevic, I. (2020). Romiplostim and eltrombopag in immune thrombocytopenia as a second-line treatment. Cureus, 12(8).
- Cabrera, F., Bressan, V., Lucero, P., Gutiérrez, I., Salvano, M., Gazzani, F. (2022). Trombocitopenia inmune primaria: reporte de casos no respondedores al tratamiento, Revista Método Investigación Aplicada a las Ciencias Biológicas, 7 (1), 37 – 41.
- Domarus, A., Farreras, P., Rozman, C., Cardelach, F., Nicolás, J., Cervera, R. Farreras Rozman. Medicina Interna (2020). Elsevier. 19na Edición.
- Donato, H., Bacciedoni, V., Rapetti, M., Lavergne, M., Rossi, N., Cedola, A. (2019). Trombocitopenia inmune. Guía de diagnóstico y tratamiento. Archivos Argentinos de Pediatría. 116 (Suplemento 6), S243 – S254.
- Fernández, S., González, J., Gálvez, E., Zubicarav, J., Sevilla, J., Sebastián, E. (2021). Manejo de la trombocitopenia inmune primaria. Comparación de dos cohortes históricas. Anales de Pediatría. 95, 86 – 92.
- Kessler, C. New strategies for the treatment of immune thrombocytopenia (2022). Clinical Advances in Hematology and Oncology. 20 (3). 151 – 153.
- Markham, A. (2018). Fostamatinib: first global approval. Drugs, 78, 959-963.
- Monteagudo, E., Astigarraga, I., Cervera, A., Dasí, M., Sastre, A., Berrueco, R., Dapena, J. (2019). Protocolo de estudio y tratamiento de la trombocitopenia inmune primaria: PTI-2018. Anales de Pediatría. 91 (2), 127.e1 – 127.e10.
- Provan, D., Semple, J. Recent advances in the mecanisms and treatment of immune thrombocytopenia (2022). eBioMedicine Part of The Lancet Discovery Science. 76.
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








