Is Fibromyalgia Related to Your Intestinal Flora?


Written and verified by the doctor Leonardo Biolatto
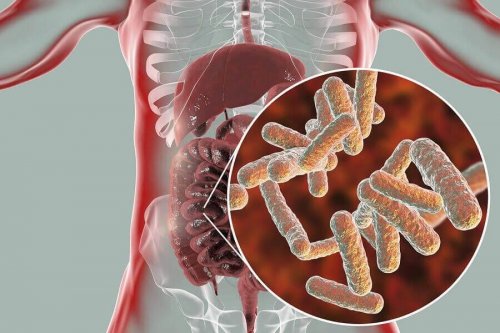
Your intestinal flora is absolutely fascinating and has been part of the most interesting research in the last few years. It’s the collection of microorganisms that live in your intestine, which includes various types of bacteria, viruses, and even fungi.
Your intestinal flora serves many indispensable purposes in your body. As many people know, these bacteria are essential to properly digest your food. But that’s not their only role in your body.
The composition of your flora can be related to many different conditions. For example, obesity. In this article, we’ll explain how fibromyalgia is related to your intestinal flora, which causes chronic pain.
What is fibromyalgia?
Fibromyalgia is a complex illness that affects about 3% of the population. In fact, it’s much more prevalent in women than in men. It’s a chronic condition that’s characterized by generalized muscle and skeletal pain.
The pain doesn’t have any observable cause. Additionally, it’s normally accompanied by tiredness, insomnia, and mood swings. The cause seems to be a change in the way the brain processes painful stimulants, which causes them to intensify.
Doctors have observed situations that trigger typical symptoms of fibromyalgia in many patients. For example, they have observed that stress or infections can trigger it. However, until relatively recently, they had never noticed a relationship with intestinal flora.
How is fibromyalgia related to intestinal flora?
As we already mentioned, your intestinal flora is made up of all the microorganisms that inhabit your digestive system. They are bacteria, fungi, and viruses that have a close relationship to your body.
In the last few years, researchers have demonstrated that your intestinal flora interacts with your body. That is, the composition of your flora has an impact on many aspects of your health. Because, in essence, each person has a different composition.
A study carried out at McGill University focused on observing the intestinal flora of people with fibromyalgia. For the study, they used samples from 156 women, 77 of whom suffered from fibromyalgia.
What they did was study the species of bacteria living in the intestinal flora of each one of the patients. Likewise, they tried to determine which bacteria had higher and lower concentrations in each person.
You might be interested in: Fibromyalgia Treatment Tips to Know
What did they observe in the intestinal flora of people with fibromyalgia?
While studying all of these people, they observed many differences in the composition of intestinal microorganisms in the people with fibromyalgia. First, what they noticed was that the symptoms of the illness were related to a change in the proportion of the bacteria.
Likewise, they observed that the intensity of the symptoms could be related to the intestinal flora. That is, there was a larger amount of certain bacteria in people who suffered a lot of pain and fatigue, for example.
The problem with the study is that it’s still not clear if the changes in intestinal microbiota cause fibromyalgia, or if they’re just a characteristic of the illness. In fact, the study was more focused on the pain symptoms. They still need to investigate whether the same changes in intestinal flora happen in other diseases with chronic pain. That way they’ll be able to see if it’s really related.

You might like to read: Is There a Connection between Gluten and Fibromyalgia?
What does it mean that intestinal flora and fibromyalgia are related?
The fact that your intestinal flora could be related to fibromyalgia opens a wide range of possibilities. For example, researchers could develop treatments and new diagnostic methods that help people to better control the illness. In fact, people are currently using intestinal flora modification to treat some conditions. Additionally, fibromyalgia is an illness that can be truly incapacitating, so this connection provides hope for the future of patients with the disorder.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- García-García-de-Paredes, A., Rodríguez-de-Santiago, E., Aguilera-Castro, L., Ferre-Aracil, C., & López-Sanromán, A. (2015). Trasplante de microbiota fecal. Gastroenterologia y Hepatologia, 38(3), 123–134. https://doi.org/10.1016/j.gastrohep.2014.07.010
- Minerbi, A., Gonzalez, E., Brereton, N. J. B., Anjarkouchian, A., Dewar, K., Fitzcharles, M.-A., … Shir, Y. (2019). Altered microbiome composition in individuals with fibromyalgia. PAIN, 160(11), 2589–2602. https://doi.org/10.1097/j.pain.0000000000001640
- Malatji, B. G., Meyer, H., Mason, S., Engelke, U. F. H., Wevers, R. A., van Reenen, M., & Reinecke, C. J. (2017). A diagnostic biomarker profile for fibromyalgia syndrome based on an NMR metabolomics study of selected patients and controls. BMC Neurology, 17(1), 88. https://doi.org/10.1186/s12883-017-0863-9
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.








